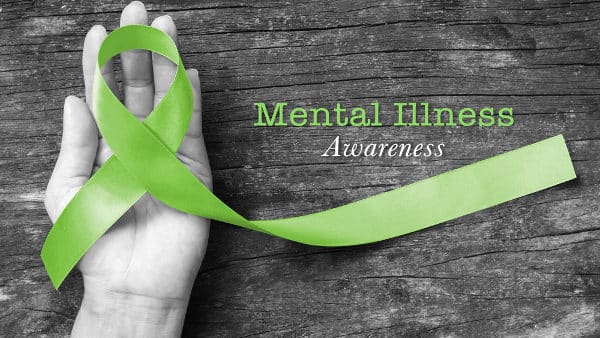
Mental health stigma remains a formidable barrier in healthcare, even as public conversations about mental wellness have become more mainstream. Many patients still hesitate to discuss their psychological struggles, and healthcare providers sometimes feel unprepared to address these complex needs.
Tens of millions of people in the U.S. deal with mental illness each year, according to the National Institute of Mental Health (NIMH). “Mental health has really worsened in recent times and the lack of its treatment and control has claimed countless human lives,” writes one GP on Sermo. Estimates suggest that only half receive treatment, according to NIMH.
Sermo poll data highlights some patient reluctance around mental health discussions. While the majority of physician respondents indicated that their patients bring up healthcare concerns on their own daily or weekly, 20% said it only happens a few times a month, and 15% indicated that they “rarely” hear their patients bring up their mental health.
An OBGYN on Sermo believes healthcare professionals should do their part to ensure patients receive mental health treatment when needed. “I feel mental health needs to be openly discussed and all patients should have a checklist ticked while taking their vital signs right from the nursing station,” they write. This article will help physicians to understand why patients may still be reluctant to speak about their mental health and how to start that conversation.
Why mental health stigma still prevents patients from speaking up
Patients can be reluctant to discuss mental health concerns due to a variety of factors. Mental health stigma manifests in three forms: public stigma, self-stigma, and structural stigma.
- Public stigma continues to cast mental health conditions as character flaws rather than medical conditions deserving treatment. These negative attitudes come from other people, which can include healthcare providers.
- Self-stigma occurs when individuals internalize society’s negative messages about mental illness. This internal dialogue can convince patients they’re fundamentally flawed, leading them to avoid seeking help altogether. Cultural factors compound these challenges, particularly in communities where seeking professional help contradicts values of family strength, emotional restraint or avoiding public shame.
- Structural stigma refers to laws, regulations, or policies that limit the rights of people with mental health conditions.
All three types can block patients from communicating openly with their providers. Mental health stigma is “a complex issue that affects individuals in various ways—whether through societal judgment, personal self-stigma, or systemic obstacles within healthcare systems,” writes a GP on Sermo.
An internal medicine physician shared their experience on Sermo. “Many patients will outrightly reject the need to be reviewed by a mental and behavioral physician even when they have florid symptoms of mental disorder,” they write. “However, dedicated counseling and sustained motivation has help me overcome this resistance as many of them eventually succumbed to be treated. Such patients do have an excellent outcome in their overall management.”
How physician preparedness affects patients’ mental health
When physicians feel prepared and unhurried, patients are more likely to share their concerns openly and honestly. Research demonstrates that patients who trust their providers have increased satisfaction with their care, better adherence to treatment and have better health outcomes. Physician attitudes toward mental health can be influenced by their own biases and training experiences.
Physicians should view these interactions through a lens of empathy, believes one internal medicine physician on Sermo. “When considering the stigma associated with mental illness and what can be done to do away with all that is associated with the unjust beliefs, it is imperative that as clinicians we interact with patients suffering from a psychological condition with the same empathetic attitude as a patient with a physical malady or any other medical condition he or she may present with,” they write.
Addressing physician preparedness requires understanding cultural sensitivities, recognizing when referrals are appropriate and maintaining therapeutic relationships that encourage ongoing dialogue. Some physicians on Sermo believe they have room for improvement. In a recent poll, 51% said they’re very comfortable discussing mental health with their patients, 35% said they’re somewhat comfortable and 12% don’t feel comfortable.

How routine mental health checks can break down stigma
Routine mental health screening represents one of the most effective strategies for normalizing mental health conversations in clinical practice. Tools like the PHQ-9 (Patient Health Questionnaire-9), GAD-7 (Generalized Anxiety Disorder-7) and ACEs (Adverse Childhood Experiences) questionnaires can uncover undiagnosed conditions before they escalate into more serious problems.
However, barriers like time constraints and insurance coverage limitations can stand in the way of routine screening. In a poll on Sermo, only half of respondents said they routinely screen patients for mental health concerns.
Some members have shared their hesitations around more frequent screening. “Many physicians without a background in psychology often avoid discussing symptoms that suggest mental illness during consultations,” writes a pediatrician. “This is usually because we feel less equipped to manage these complex issues. We may worry about making inaccurate assessments or not having the appropriate resources to help.”
“Although this is a very important topic that we should discuss with our patients, with so little time allocated for their visits and so many other important medical issues, mental health needs tend to be a lower priority,” adds an OBGYN.
Others have imported their peers to use screening more regularly. “Mental health is so important even for non-psych specialties like mine,” writes an infectious disease specialist. “It totally affects how patients receive and implement their treatment recommendations! We need to do more as a health system to address this!” A GP says they “encourage everyone to try it,” while a family medicine physician thinks “people are becoming more comfortable discussing these issues with their doctors, so we need to stay updated to meet those needs.”
What’s being done to reduce mental health stigma & what else is needed
Numerous successful stigma-reduction initiatives have emerged across healthcare systems and communities. Programs like Mental Health First Aid provide training for healthcare providers and community members to recognize mental health crises and provide support. Anti-stigma training programs help healthcare workers examine their own biases and develop more supportive approaches to patient care. However, Sermo data suggests physicians aren’t necessarily aware of these programs’ existence. In a poll, the majority of respondents indicated that they’re not aware of any programs for reducing mental health stigma. The most widely known program was Stop Stigma Together, which received 14% of votes.
Public awareness campaigns set out to reduce stigma and encourage help-seeking behavior. These initiatives often feature personal stories from individuals who have successfully managed mental health conditions, helping to humanize mental illness and reduce fear.
Trauma-informed care models represent another important development in stigma reduction. These approaches recognize the widespread impact of trauma and integrate this understanding into all aspects of patient care. By acknowledging how past experiences affect current health, trauma-informed care reduces blame and judgment while promoting healing.

Transforming mental health care through physician leadership
Mental health stigma continues to create significant barriers to patient care, preventing individuals from seeking necessary treatment and contributing to poor health outcomes. Lingering stigma could be contributing to delayed treatment, reduced treatment adherence, and social isolation.
Physicians hold a unique position in society to address and reduce mental health stigma. Through their daily interactions with patients they can drive meaningful change in how mental health conditions are perceived and treated. Key strategies for physicians include:
- normalizing mental health discussions during routine patient encounters
- implementing routine screening protocols when feasible
- examining and addressing personal biases about mental health
- supporting colleagues experiencing mental health challenges, and
- advocating for improved mental health resources and policies within their organizations.
Healthcare providers have the opportunity to lead by example, showing patients and communities that mental health deserves the same attention and care as physical health. As one family medicine physician shares, “I’ve found that mental health often plays a significant role in the physical symptoms that bring patients to my practice. By addressing mental health openly, I can help patients understand the connection between their emotional well-being and physical symptoms, fostering a more holistic approach to their health. This also allows me to build trust with patients, encouraging them to share concerns they might otherwise keep hidden, which is essential for providing comprehensive care.”
The Sermo community represents a powerful platform for driving this change. Join the conversation on Sermo to connect with colleagues who are working to reduce mental health stigma and improve patient care. Together, we can create a healthcare system where mental health stigma no longer prevents patients from receiving the care they need and deserve.