What seemed rooted in science fiction just 100 years ago is now an integral part of modern medicine: robotics in surgery. Robotic surgery’s literature and applications are expanding quickly in real-time, with promising potential for all specialties.
Let’s explore the benefits of robotic surgery, the most common robotic surgery procedures and the factors concerning current and future trends.
What is robotic surgery?
Robotic surgery refers to a surgeon’s use of robotic systems to perform surgical procedures. These procedures are minimally invasive and can allow for more precision than traditional open procedures.
Patients and even medical professionals have misconceptions about how robotic surgery is done. One Sermo member says, “Most patients and many doctors think that you just press a button on the laser to do cataract surgery and that they are all the same and the surgery requires no skill.” The technology used in robotic surgery is better thought of as a tool that the surgeon uses to perform the surgery with more accuracy, smaller incisions, and better ergonomics.
The history of robotics in surgery
The role of robotics in medicine has evolved exponentially since its inception. One physician on Sermo shares, “The technology behind robotic surgery is incredible. I started performing robotic surgeries in the mid-90s when the intuitive surgical system first hit the market.”
In 1985, Dr. Yik San Kwoh performed neurosurgical biopsies using the Programmable Universal Machine for Assembly 200 (PUMA), marking the first time a surgeon used a robotic platform on a human patient. Professor Brian Davies of Imperial College London soon after adapted PUMA for urologic and prostate procedures.
In 1994, AESOP 1000—the first robotic arm model—gained FDA approval. Four years later, Computer Motion introduced the ZEUS system, offering surgeon-controlled arms and instruments. That same year, surgeons at the Cleveland Clinic first used the ZEUS platform for a uterine tube anastomosis procedure.
In 2001, Operation Lindbergh marked a major milestone in robotic surgery: surgeons used the ZEUS robot and the SOCRATES telecollaboration system to perform a cholecystectomy in Strasbourg, France, from New York. Jacques Marescaux conducted the 54-minute procedure without technical issues or noticeable delay.
Around the same time (2000), the FDA approved the first da Vinci robot—now one of the most common in the business. It featured three arms: one for the endoscope and two for instruments. In 2002, recognizing the benefits of an extra instrument, the FDA approved a four-arm version.
Skip forward to today, and industry leader Intuitive Surgical’s latest and most advanced model—da Vinci 5—surpasses previous models in advanced imaging, enhanced instrument dexterity and improved ergonomics. Other robotic tools closely match da Vinci 5, with the medical devices industry growing increasingly competitive.
Advantages of robotic surgery: 3 benefits
Emerging trials indicate that robotic-assisted surgery improves patient outcomes, reduces hospitalization length and decreases surgeon fatigue. Here’s a deeper look into the pros of robotic surgery:
1. Improved patient outcomes
Robotic-assisted surgery reduces both intraoperative and postoperative complications. For example, data from 18 randomized controlled trials shows that compared to open radical prostatectomy, robotic-assisted radical prostatectomy yields fewer biochemical recurrences and short-term improvements in quality of recovery and pain (up to six weeks postoperatively).
2. Reduced length of stay
Robotic surgery often leads to shorter hospital stays than traditional open surgery. This extends to reduced hospitalization costs.
A trial involving 29 surgeons across nine UK hospitals found that patients who received robot-assisted surgery (specifically, a procedure known as cystectomy) stayed in the hospital for an average of eight days—two days fewer than traditional open surgery. The study also indicated that robotic-assisted surgery achieved a 52% reduction in readmission rates.
3. Decreased surgeon fatigue
Fatigue closely correlates with surgical errors. Robotic surgical systems help reduce fatigue among surgeons through ergonomic enhancements, minimal instrument movement restrictions, comfortable seating and stable visualization, putting less pressure on the cervical spine.
For example, robotic surgery research published in the Journal of Gastrointestinal Surgery demonstrates that, compared to standard laparoscopy, robot-assisted procedures consistently lower muscle activation (measured by EMG) and reduce mental workload (measured by NASA-TLX and heart rate). This means doctors have more energy and better outcomes.

3 trends in robotics for surgeons
The literature and applications surrounding surgical robots are growing quickly. Here’s a look into three trends in this space and the future of robotic surgery:
1. Miniaturized robotic systems
Miniaturization offers marked advantages over open surgery. Miniaturized robotic systems can be deployed in any standard operating room—eliminating the need for a dedicated “robot room”—and their reusable, easily sterilizable design streamlines setup, enabling faster procedures and quicker turnover for patients and operating staff.
In a prospective study published in Diseases of the Colon & Rectum, 30 patients undergoing right or left colectomy with a miniaturized robotic surgical system experienced no conversions to open surgery, no system-related adverse events and a low overall morbidity rate. Additionally, patients’ median hospital stay was only two days compared to a median of 6 days for open colectomy.
2. Artificial intelligence and machine learning
Artificial intelligence (AI) and machine learning (ML) are revolutionizing robotic surgery across specialties. Let’s explore a handful of use cases:
Patient-specific implant positioning in knee/hip arthroplasty
The MAKO robotic system leverages AI to convert preoperative CT scans into 3D joint models. Its ML algorithms optimize implant size, alignment and ligament balance during total knee and hip replacements.
Research published in PLOS One demonstrates the technology’s improved component positioning accuracy, having reduced glenoid malposition from 68.6% to 15.3% in shoulder arthroplasty.
AI-guided 3D augmented reality (AR) in kidney transplantation
AI computer vision modules process preoperative CT scans to generate 3D reconstructions of the recipient’s vasculature. Intraoperatively, AR overlays these reconstructions onto the robotic console’s view, aligning with real-time instrument tracking and allowing for more accurate movements.
AI-enhanced glenoid component placement in shoulder arthroplasty
For total shoulder arthroplasties, AI software merges preoperative CT or MRI data with real-time tracking. It guides robotic arms in preparing the bone and placing glenoid implants based on existing images of the joint.
3. Telesurgery
The newest frontier in robotic surgery is telesurgery, or the ability to perform surgery remotely using a console in one location with the robotic arms performing the surgery in a separate location. Globally, the current systems with telesurgery potential include the following:
Hinotori
Hinotori is a multi-port, single-boom robotic-assisted surgery system. In August 2020, Japan’s Pharmaceuticals and Medical Devices Agency (PMDA) approved hinotori for urology. By October 2022, its approval expanded to gynecology and general surgery.
Two comparative studies—one published in the Journal of Robotic Surgery, and the other in the Journal of Endourology—with the da Vinci system for partial nephrectomy and radical prostatectomy found no differences in peri-operative outcomes.
KangDuo
SuZhou KangDuo Robot Co. created the KangDuo Surgical Robot System (KD-SR-01) as a robotic surgery system for urological procedures.
A prospective randomized trial of 100 patients found the KangDuo system to be non-inferior to the da Vinci system for partial nephrectomy in T1a lesions. Another comparison of da Vinci and KangDuo for robot-assisted radical prostatectomy reported similar short-term oncologic and functional outcomes, though operation time was longer with KangDuo.
Microport Medbot
MicroPort MedBot Robotic Systems comprise multiple robotic-assisted surgery platforms, and Toumai from MicroPort has the largest series of telesurgery procedures in humans. During a laparoscopic spermatic vein ligation procedure at Xinjiang Kezhou People’s Hospital, a surgeon at the Telemedical Center of the First Affiliated Hospital of Nanjing Medical University—nearly 3,800 kilometers away—controlled the console.
4 common robotic surgery procedures
A physician on Sermo explains, “Urologic, thoracic procedures and gynecology procedures are being done robotically and are actually done quite well with the robotic system.” For more context, here are some robotic surgery examples and common procedures:
1. Gynecologic surgery
Surgeons commonly perform robotic-assisted hysterectomies. A meta-analysis published in the Journal of Robotic Surgery indicates that robotic-assisted hysterectomy is associated with a shorter hospital stay, reduced blood loss and fewer complications compared to open surgery.
2. Urologic surgery
Research published in Medical Science Monitor shows that robotic-assisted prostatectomies result in lower blood loss, reduced transfusion rates and a higher rate of nerve-sparing procedures compared to laparoscopic and open prostatectomies.
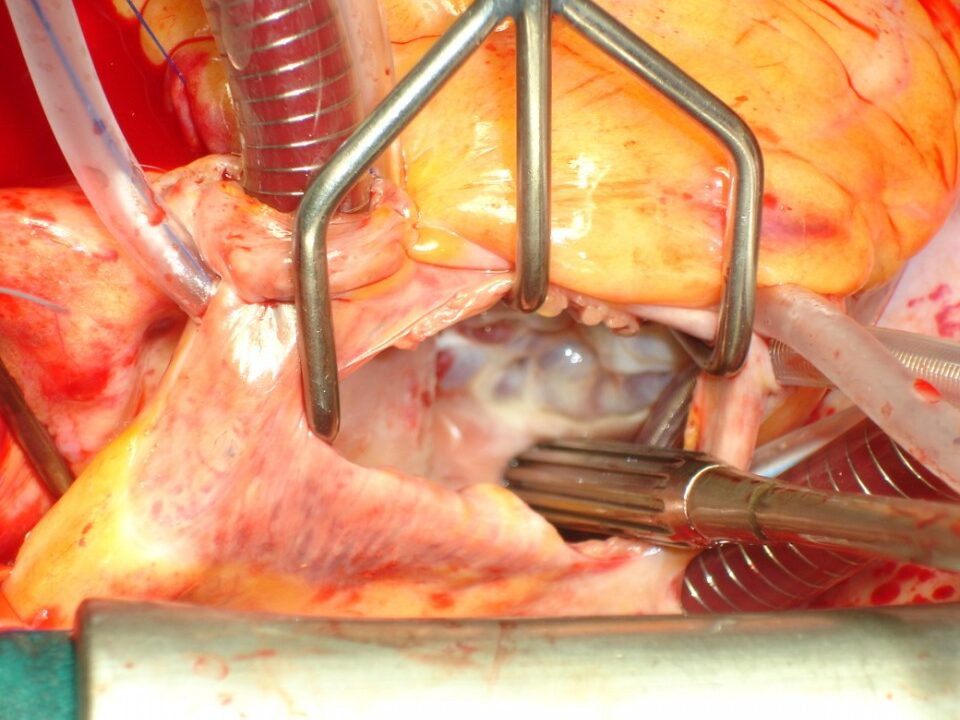
3. Cardiac surgery
One group of researchers found that, in terms of safety, robot-assisted mitral valve repair is comparable to conventional sternotomy and other minimally invasive procedures. But researchers note the technology’s advantages in reduced atrial fibrillation, shorter ICU and hospital stays, less pain and quicker recovery times.
4. Orthopedic Surgery
Research published in the Journal of Clinical Medicine associates robotic-assisted total hip arthroplasties with improved radiological outcomes, particularly in acetabular component positioning. It also associates robotic assistance with reduced rates of leg length discrepancy. However, functional outcomes between robotic and conventional THA remain equivocal, with no consistent advantage in patient-reported outcome measures.
Will robots replace surgeons?
The use of robots doing surgery and other procedures is growing. Analysts anticipate the market for robotic surgical devices to grow from $7.84 billion in 2024 to $8.89 billion in 2025, at a 13.4% compound annual growth rate.
But a burgeoning field doesn’t mean a takeover. Robotic systems are non-autonomous, which means they need human surgeons and experts to operate. While the future of robotic surgery is uncertain, we can expect these systems to remain human-dependent for the foreseeable future.
Additionally, robotics doesn’t work for every specialty. A physician on Sermo shares, “I am a general bariatric surgeon and really found that the robotic surgery actually slowed me down and ended up costing a lot more per case. Other specialties are different.” And according to a Sermo poll, only 8% of physicians use robotics in their practices whereas technologies like AI and telemedicine are more common.
Learn how other physicians view robotic systems by joining Sermo
Whether you’re curious about the role of robotics in fields other than your own or want to hear about fellow professionals’ opinions, join Sermo.
Sermo is the largest community of physicians in the world. Physicians can communicate on the topics that matter most to them—and their patients. Join the conversation with 1.5 million other doctors on robotic surgery’s evolving literature, and have a few laughs along the way.
Frequently asked questions
Is robotic surgery better than traditional surgery?
Robotic surgery versus traditional surgery isn’t much of a debate. Robotic surgery isn’t “better” or “worse” than traditional surgery, but tools to consider. For certain procedures, researchers associate robotic assistance with reduced hospitalization duration, lowered costs and improved patient outcomes.
Is robotic surgery safe?
Risk varies depending on the procedure. While the majority of robotic-assisted surgeries have markedly low complication rates, certain evolving technologies—like telesurgery—may introduce more risk.
Can robots perform surgery without a surgeon?
The main disadvantage of robotic surgery is that it still requires human oversight. While robotic systems’ autonomy is increasing as technology advances, we’re yet to see the first fully autonomous surgical system.