If you knew of a newly developed prevention method that offered your patients 90% protection from a potentially fatal and incurable viral infection, would you offer it to them?
HIV experts are more optimistic than ever that there may finally be an effective strategy to stop the 35-year old pandemic from spreading further. Even though a vaccine has yet to materialize, researchers have found that newer tools such as Treatment as Prevention (TasP) and Pre-Exposure Prophylaxis (PrEP) are 90% effective at inhibiting the spread of HIV. Let’s look at what got us to this point, and where the future may lead.
Slow, Steady Progress
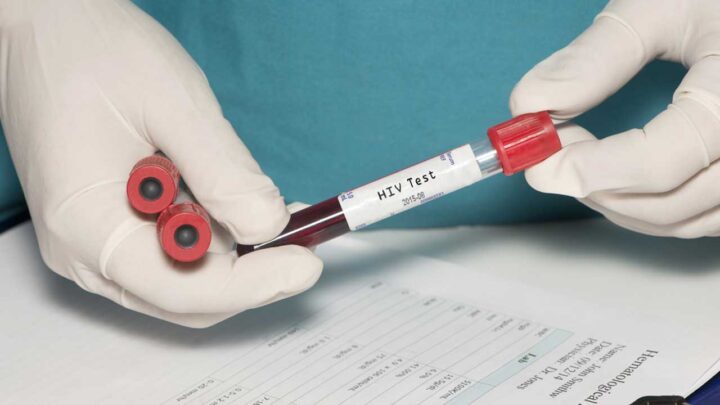
Interestingly, one of the earliest weapons in the fight against the spread of HIV—reliable and readily-available routine HIV testing—has helped reduce the percentage of undiagnosed HIV infections from 20% in 2008 (MMWR: HIV Surveillance United States, 1981—2008) to 13% in the most recent Centers for Disease Control and Prevention (CDC) report. National HIV Testing Day, June 27, should serve as a reminder for health care providers and patients alike that HIV testing is a critical starting point to help identify new infections and link individuals to care. Additionally, in the case of negative results, testing can serve to jump-start conversations about risk reduction and prevention methods.
Along with testing, providers should revisit prevention methods that aren’t often in the news, but are still an essential part of a comprehensive approach. This includes the consistent use of condoms; routine screening for sexually transmitted infections (STIs); post-exposure prophylaxis with anti-retroviral therapy; and behavioral counseling to discuss safer sexual behaviors, partners’ HIV status, and reducing patients’ number of sexual partners.
A Pair of Potent New Tools
In addition to these tried-and-true tools, an ever-expanding body of evidence has helped researchers and providers develop other prevention methods with high efficacy and scalability that may further stem the tide of new infections.
For example, the HPTN 062 trial showed that TasP reduced HIV transmission within serodiscordant couples by 96% (Cohen, M et al, NEJM). Ongoing trials designed to pinpoint just how infectious a patient with an undetectable HIV viral load is to their partners have yielded estimates quite close to zero (PARTNER study; Rogers et al). With better engagement, retention, and provision of anti-retroviral therapy for those living with HIV, transmission is predicted to decrease to very low levels (Montaner J et al).
The latest addition to the prevention toolkit has taken a while to catch on, perhaps because it requires a paradigm shift from traditional methods. In 2012, the FDA approved PrEP, which is the provision of anti-retroviral drugs to HIV-negative at-risk individuals. PrEP offers a key advantage over other methods: it places control in the hands of the HIV-negative individual, who may not otherwise exert pressure on a sexual partner to use another prevention method.
PrEP has proven effective in clinical trials and real-world demonstration projects. Importantly, its effectiveness varies widely with medication adherence, from 44% in trials with low levels of adherence to greater than 90% in trials with higher levels.
PrEP: A “How to” Guide
The Centers for Disease Control and Prevention have published a Clinical Practice Guideline for HIV Pre-exposure Prophylaxis to help primary care providers integrate PrEP into their comprehensive prevention activities. To briefly summarize, PrEP involves three steps:
- Assessment. Providers should perform a baseline clinical assessment—including a detailed sexual history and risk factors for HIV acquisition—to identify PrEP candidates. PrEP is indicated for partners of HIV-positive patients, and individuals at risk of acquiring HIV through sexual activity or drug use. Baseline labs should include an HIV test to ensure HIV negative status, screening for viral hepatitis, and an assessment of renal function. If a recent high-risk exposure has occurred, an assessment should be made of the likelihood of acute HIV infection.
- Prescription. Providers should give patients a limited PrEP prescription (a 90-day supply to ensure the patient returns for HIV testing) with proper counseling. The only currently approved PrEP agent is the fixed-dose combination of Emtricitabine/Tenofovir DF, taken once daily with food.
- Follow-up. Providers should follow up with patients at 3 months to monitor HIV status, pregnancy, risk behaviors, side effects, adherence, and ongoing indications for PrEP. At least every 6 months, renal function should be monitored and patients should be screened for STIs.
Getting to Zero
Combination prevention—making HIV-positive individuals virtually non-infectious with anti-retroviral therapy and providing effective prophylaxis and other comprehensive prevention methods to those at high risk—has the potential to dramatically decrease new infections. Organizations in New York and California are doing their part to spread the word about the potential of these efforts to curb new infections.
Bringing Prevention Home
The great strides of the past 35 years have brought us to a unique moment. Armed with potent prevention tools for those who already infected as well as those at risk, we can now envision a future in which new HIV infections are rare.
But this future will require the extensive efforts and cooperation of all providers, from specialists to primary care. Otherwise, we may fall victim to a “knowledge-implementation gap” in which we know what to do, but lack the will do to it.
It starts with an open and honest sexual history, involves frequent HIV testing, and continues with combination prevention, including anti-retroviral TasP, STI testing, provision of condoms, and PrEP. Although prescribing PrEP may take some extra effort, every patient in every primary care setting deserves access to evidence-based HIV prevention.
This HIV Testing Day, join the effort to usher in an AIDS-free generation.