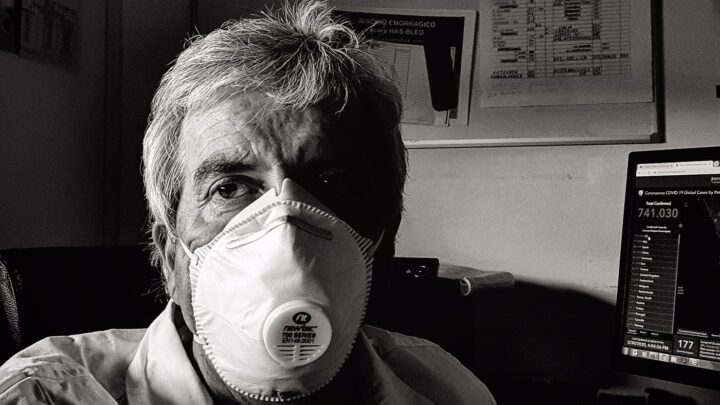
Physician burnout isn’t just about feeling tired after a long shift, it’s a profound state of emotional, physical, and mental exhaustion that affects how physicians view their profession and themselves. The issue is widespread, affecting an estimated 45.2% of physicians in the U.S., according to a 2023 survey of more than 7,600 participants published in Mayo Clinic Proceedings.
Burnout rates among physicians are significantly higher than in other professions, the survey found. While burnout is cause for concern in any field, in medicine it’s especially critical. When doctors feel burnt out, patient care quality deteriorates, medical errors increase and healthcare systems face high turnover costs.
Among the Sermo community, 53% of respondents in a poll indicated that they feel overworked “all of the time” or “most of the time.” If you’re in that camp and ready to make a change, your medical degree and clinical experience have prepared you for far more than traditional patient care. A world of fulfilling alternative careers awaits—routes that leverage your expertise while offering better work-life balance and renewed professional satisfaction.
Understanding the roots of physician burnout
Staff shortages are a major cause of physician burnout, as indicated by feedback from the Sermo community. In a poll, 56% of respondents said they’re currently understaffed, and an additional 27% said they’ve previously been short staffed.
“Short staffing has a huge effect on burnout,” one general practitioner on Sermo writes. “Physicians are prone to mistakes, can suffer from mental issues, fall ill, etc.”
It creates a vicious cycle, according to another GP on Sermo. “Burnt out staff leads to increased absences which further increases the pressure,” they write. “When you feel supported you can tolerate an amazing amount of pressure/stress/challenges and lift each other up—a challenging environment can create a wonderful sense of community and camaraderie when you know your team has your back… And sadly this is what is being chipped away.”
Physicians are then left to face high administrative burdens under the mounting pressure.
Multiple factors can contribute to physician burnout. Administrative burden is a major contributor, with doctors spending managing heavy workloads without adequate support, according to one study. Electronic health record (EHR) systems, originally designed to improve efficiency, unintentionally created heavier workloads for physicians, according to the study.
The study authors also mention loss of autonomy. Physicians who entered medicine to heal and help patients find themselves constrained by insurance protocols, hospital policies and productivity metrics that prioritize quantity over quality. The moral injury of being unable to provide optimal care due to system limitations creates deep professional dissatisfaction.
Long hours remain endemic to medical culture, despite mounting evidence of their harmful effects. This can lead to chronic sleep deprivation and deteriorating personal relationships, according to the study. The emotional toll of constantly confronting suffering, death, and human tragedy—without adequate support systems—creates compassion fatigue.
In some instances, physicians can find better support without leaving clinical practice. “My previous organization had a lot of turnover in support staff which led to a lot of challenges with workload,” writes a GP on Sermo. “My current organization offers some hiring incentives for support staff as well as having competitive pay and hours to retain clinicians.”
For those who would prefer to transition to an alternative career path instead, multiple options exist for consideration.
Alternative career paths for burnt-out physicians
The good news if you’re experiencing burnout is that your medical training has equipped you with skills highly valued across numerous industries. These are the most promising non-clinical career paths that allow you to leverage your expertise without traditional practice pressures.
Healthcare consulting and pharmaceutical industry
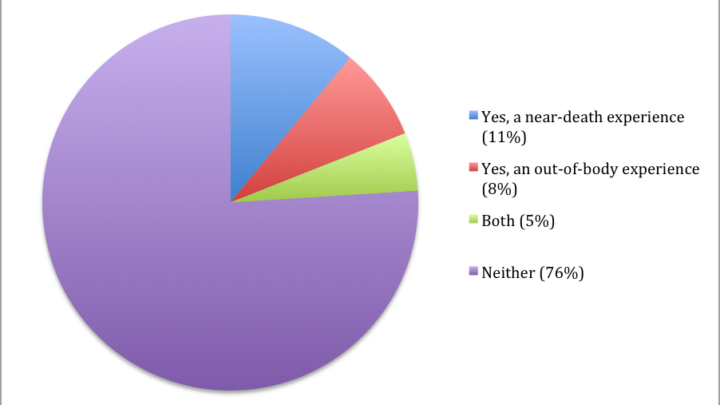
In an internal Sermo poll, healthcare and pharmaceutical consulting emerged as the most popular career alternative, with 53% of participants indicating that it’s the career path they’d be most interested in if they were to leave clinical medicine (note: members could select more than one answer). Healthcare consulting offers physicians the chance to influence healthcare delivery on a larger scale. Management consulting firms like McKinsey, BCG and Bain recruit physicians for their healthcare practices.
Pharmaceutical companies offer numerous roles including medical affairs, clinical development, regulatory affairs and market access. These positions can provide a better work-life balance than clinical practice, and the median total pay for a pharmaceutical consultant in the U.S. is $156,000, according to Glassdoor data.
Telemedicine and part-time clinical roles
The second most popular career alternative among polled Sermo members was telemedicine or part-time roles, accounting for 48% of responses. Telemedicine roles span primary care, specialty consultations, urgent care and chronic disease management, often with more reasonable hours than traditional practice.
For physicians wanting to maintain some clinical connection while reducing burnout, telemedicine offers flexibility and better work-life balance, as one emergency medicine physician on Sermo can attest. “My telemedicine career actually started with working as a collaborating physician for Acne/Anti-Aging Telemedicine practice with Curology,” they write. “I was already getting burned out from the Emergency Dept after 10 years and telemedicine provided an opportunity to cut down from the ED. Of course the compensation was less but my mental health was so much better. Further, the flexibility was a welcome addition.”
Entrepreneurship and healthcare innovation
Physicians make natural entrepreneurs in the healthcare space, understanding market needs and pain points from firsthand experience. Successful physician entrepreneurs have launched everything from medical device companies to health tech startups. 34% of participants in the poll voted that they’d be interested in entrepreneurship or starting a business.
Teaching and academic research
When physicians take up academic medicine without clinical responsibilities, it can reignite their passion for the intellectual aspects of medicine. Opportunities include medical school teaching, curriculum development, educational research and administrative roles in medical education.
A portion of physicians on Sermo are interested in this path to shaping the next generation of healthcare providers and conducting research that improves healthcare delivery. 22% of poll participants voted for teaching and academic research as the career option they’d be most interested in.
Medical writing and communications
Medical writing represents another accessible transition for physicians. Your clinical background provides credibility and deep understanding that non-physician writers can’t match. Opportunities span regulatory medical writing for pharmaceutical companies, medical journalism, continuing medical education content creation and health marketing communications.
Regulatory medical writers in the U.S. earn between $102,000 to $148,000 annually, per Glassdoor data. The work involves creating clinical study reports, subject narratives and package inserts, tasks that draw directly on your clinical research knowledge.
Public health and policy
For physicians motivated by population health improvement, careers in public health offer meaningful work. Opportunities exist in government agencies, NGOs, think tanks, and advocacy organizations.
Roles include epidemiologist, health policy analyst and public health administrator. Each leverages your medical knowledge while focusing on prevention and system-wide improvements rather than individual patient care.
Leveraging your medical expertise in alternative roles
To land a new role, you’ll need to be able to recognize and articulate your transferable skills. These are some of the capabilities that’ll make you stand out.
- Critical thinking and problem-solving: medical diagnosis requires analyzing complex, ambiguous information under pressure to make high-stakes decisions. This skill translates directly to business consulting, research and strategic roles.
- Leadership and team management: you may lead multidisciplinary teams, coordinate care across specialties, and make decisions affecting multiple stakeholders. These experiences prepare you for management roles in any industry.
- Communication skills: you build communication skills while explaining complex medical concepts to patients and their families. Whether writing regulatory documents, presenting to executives, or teaching – your communication skills are transferable.
- Scientific rigor: your training provides a strong foundation for roles requiring analytical thinking and data interpretation.
- Empathy and emotional intelligence: clinical practice develops deep empathy and ability to navigate emotionally charged situations—skills valuable in consulting, management and customer-facing roles.
- Adaptability and continuous learning: medicine’s rapid evolution requires constant learning and adaptation to new technologies, treatments, and guidelines. This serves you well in any field undergoing change.
When positioning yourself for non-clinical roles, it helps to frame your medical experience in business terms. Instead of “managed patient care,” describe “led cross-functional teams to deliver optimal outcomes under resource constraints.” Rather than “clinical experience,” highlight “stakeholder management and crisis resolution in high-pressure environments.”
Emphasize outcomes and metrics where possible. Quantify your experience: “Managed care for 20+ patients daily,” “Reduced diagnostic errors by implementing systematic protocols,” or “Led quality improvement initiatives resulting in 15% efficiency gains.”
Navigating a career transition: practical steps
Here’s a step-by-step approach to landing a new role.
- Self-assessment and goal setting: identify your core motivations—are you seeking better work-life balance, intellectual stimulation, financial growth, or societal impact? Use career assessment tools (such as those from the Association of American Medical Colleges) and consider working with a career coach who specializes in physician transitions.
- Research and networking: conduct informational interviews with physicians who have made similar transitions. The Sermo community, for example, is an invaluable tool for connecting with physicians in alternative careers. You could also join physician career transition groups, attend relevant conferences and participate in professional associations in your areas of interest. The American Medical Writers Association, Healthcare Financial Management Association and similar organizations offer networking opportunities and educational resources.
- Skill development: identify skill gaps between your current capabilities and target role requirements. Consider pursuing relevant certifications or coursework, e.g., MBA programs, certificate programs in medical writing or specialized training in areas like healthcare consulting or regulatory affairs.
- Resume and LinkedIn optimization: transform your clinical CV into a business-focused resume highlighting transferable skills and quantifiable achievements. Optimize your LinkedIn profile for your target industry, incorporating relevant keywords and showcasing your unique physician perspective.
- Interview preparation: prepare compelling stories that demonstrate how your medical background provides unique value in non-clinical settings. Practice articulating your transition rationale in positive terms, focusing on what you’re moving toward rather than what you’re leaving behind. Research common interview questions for your target roles and prepare specific examples from your medical experience that demonstrate relevant competencies.
- Managing the transition: consider transitioning gradually when possible, to maintain financial security while allowing time to build new skills and networks.
Reclaiming well-being and finding renewed purpose
When you’re burnt out, it can feel as though there’s no way to dig yourself out of the hole, a radiation oncologist on Sermo argues. “It seems that practicing as a physician becomes that we have to be able to cope with everything, high workload and conditions that do not seek our well-being, when paradoxically we seek the health of our patients but sometimes it is difficult for us to find our own balance within this system,” they write.
Career transitions offer the opportunity to fundamentally reimagine your relationship with work and rediscover professional satisfaction. A new role can improve your work-life balance, stress levels and overall life satisfaction.
Consider seeking roles that align with your core values and provide meaning beyond financial compensation. Opportunities abound, since your medical expertise is highly transferable and valued across numerous industries.
As you consider your options and plan your transition, Sermo can provide a supportive community where you can connect with peers who understand your challenges. Our community offers a space to explore career options, share experiences and receive guidance from fellow physicians who have navigated similar journeys. You can use their feedback to inform your search for a role that will serve your unique goals, values and aspirations for professional renewal.