Ten years ago, a patient with puzzling shortness of breath might have faced a series of appointments, rounds of imaging and weeks of uncertainty before their physician could name the culprit. Today, that same physician can pull up an AI-flagged CT scan within minutes, cross-reference lab and genetic data in real time and arrive at a confident diagnosis before the patient leaves the room. This shift—from relying primarily on experience and intuition to leveraging a powerful suite of digital tools—has transformed not only how quickly physicians can make diagnoses, but also how precisely they can tailor treatment plans.
Recent data from the Sermo community reveals fascinating insights into how physicians are adapting to and implementing diagnostic technologies like these in their daily practice. Whether you’re a seasoned practitioner looking to expand your diagnostic toolkit or simply seeking to understand how your peers are leveraging these innovations, consider this article to be your complete overview of modern diagnostic technology.
The current landscape of diagnostic technologies
Diagnostic technology encompasses a broad spectrum of tools that enable physicians to identify, monitor and assess medical conditions. This includes everything from traditional laboratory tests and basic imaging to cutting-edge molecular diagnostics, AI-enhanced analysis and wearable remote monitoring devices.
Advanced imaging technologies
The Sermo community has highlighted the integral role that advanced imaging technologies like MRI, CT and ultrasound play across multiple specialties. “Diagnostic imaging plays a very important role in my medical practice,” notes a radiation oncologist on Sermo. “Imaging studies, such as MRI and CT, are vital for confirming diagnoses in neurology,” a neurologist similarly shared.
Modern MRI technology has evolved far beyond traditional systems. For example, wide-bore MRI systems accommodate larger patients and those with mobility limitations. CT technology continues advancing with lower radiation doses, faster acquisition times and improved image resolution. Ultrasound technology has become increasingly portable and sophisticated, with handheld devices now providing diagnostic-quality imaging at the bedside. This portability has expanded ultrasound applications across specialties, from emergency medicine to primary care.
Traditional lab tests
Sermo members also often use traditional lab tests. These include tests that have been around for decades, such as lipid panel blood tests, urinalyses to check for infection or throat swab strep tests. In the past, lab tests were mostly carried out and read manually, but now they’re now highly automated, and AI could further enhance the process by making diagnostic suggestions based on data, according to one narrative review.
It can be an affordable option relative to other tools, reveals a general practitioner. “We prefer to use traditional lab tests,” they share. “Sometimes, the cost of tests prevents patients from doing so. New diagnostic technologies are helpful if we want to investigate further.”
Point-of-care testing
Point-of-care testing has proven popular among physicians who value convenience and speed. “My current role has required me using point of care testing quite often and I find the speed and ease really helpful,” writes another GP.
Modern point-of-care devices can provide results for cardiac markers, infectious disease screening and glucose monitoring within minutes rather than hours. This immediate feedback allows physicians to initiate treatment promptly.
Genetic and molecular diagnostics
Some Sermo members have begun using personalized medicine in clinical practice, relying on tools that enable the physicians to tailor treatments based on individual patient genetic profiles and molecular characteristics. For those who incorporate them, the molecular assays and genetic panels help physicians predict drug responses, identify genetic predispositions to diseases and select targeted therapies.
The application of genetic testing extends across numerous specialties. “As a psychiatrist, I have started to incorporate more genetic testing for patients and their metabolic profile for detoxifying medications with regard to the Cytochrome P450 system,” explains one Sermo member. “I have greatly improved the sensitivity for individualized medication planning. It has greatly helped my patient outcomes.”
The testing can also be useful in pediatric medicine. “Genetic testing has become more available and precise in the last decade and has allowed for early intervention and targeted therapies for pediatric patients,” a pediatrician on Sermo notes. “Having a diagnosis provides a lot of relief and guides anticipatory management for families, which in itself can be therapeutic as well.”
Remote and wearable monitoring devices
Remote monitoring wearable devices enable continuous monitoring of vital signs, activity levels and physiological parameters when patients are outside the clinic.
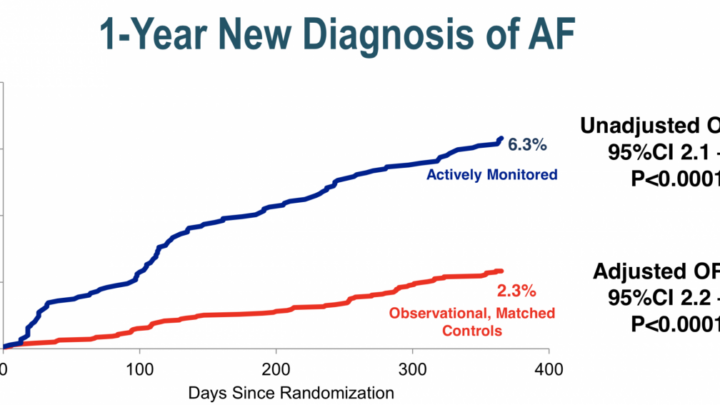
Wearable devices can track heart rhythm abnormalities, monitor glucose levels in diabetic patients and assess sleep patterns. They can also alert patients to potential health issues, encouraging them to take proactive measures.
In the past, devices such as smartwatches offered only limited tracking capabilities, such as counting steps and measuring basic heart rate but providing little clinical insight. Their data were intermittent and primarily geared toward fitness enthusiasts rather than patients.
Today’s remote monitoring devices, by contrast, have evolved into sophisticated health platforms capable of tracking a range of vital signs and physiological parameters. Examples include the Apple Watch Series 9, which can perform on-wrist ECGs and detect irregular heart rhythms; the Oura Ring, which monitors heart rate variability, body temperature, and sleep stages; and continuous glucose monitors (CGMs) like Dexcom G7 or Abbott’s FreeStyle Libre 3, which provide real-time blood glucose readings.
Challenges of diagnostic technologies
While diagnostic technologies have transformative potential, you may come across challenges implementing them.
Cost and insurance coverage limitations
In a Sermo poll, members cited financial constraints as the most significant barrier to diagnostic technology utilization, with 44% of votes. “I rely mainly on diagnostic imaging e.g. Ultrasound, CT and MRI,” notes a general surgeon and Sermo member from Nigeria. “However, the main challenge here is the cost. Not many patients can afford out-of-pocket payment.”
Insurance doesn’t always cover the latest technological advances. “Patients often request advanced lab testing when it may not be covered by insurance and may not have the evidence to support its widespread adoption,” writes a GP from the U.S. “These can be challenging and time-consuming conversations to have.”
The cost barriers are particularly pronounced in certain regions. “It is really challenging to use these new technologies, especially in developing countries, where it is difficult even to have conventional diagnostic tests,” notes a GP member from Honduras.
Some members would like to see insurance coverage decisions catch up. “The greatest challenges has been raising awareness of these tests and improving access and insurance coverage of them, given the cost and logistical barriers involved,” stresses a radiologist from the U.S.
Access to up-to-date equipment
13% of survey respondents indicated that their main barrier was a lack of access to up-to-date equipment. The rapid pace of technological advancement can create situations where existing equipment becomes outdated, requiring significant capital investments to maintain current diagnostic capabilities.
This challenge is particularly prevalent in low-resource settings, where physicians may be limited to using outdated equipment donated by higher-resource areas. And while some rural areas have embraced telemedicine, others lack access to basic broadband connectivity.
Integration with electronic health records
Electronic health record (EHR) integration challenges affect 12% of voters, highlighting the complexity of incorporating new diagnostic technologies into existing healthcare information systems. Seamless integration is crucial for maintaining efficient workflows. Poor integration can create workflow disruptions, duplicate data entry requirements and exacerbate communication gaps that compromise patient care.
Interpretation complexity and training needs
Interpretation complexity and training requirements represented 11% of votes. Diagnostic tools can require specialized knowledge for accurate interpretation and clinical application.
An internal medicine physician on Sermo provides an example: “It can be challenging to remember the PPV, NPV, etc., of different lab tests, especially if subtleties influence them in the patient’s characteristics/presentation.”
Patient acceptance and compliance
Patient acceptance and compliance issues affect 5% of physicians who responded in the poll. Some patients may be hesitant to undergo newer diagnostic procedures due to unfamiliarity, cost concerns or anxiety about potential results.
Remote monitoring and wearable devices require ongoing patient engagement and compliance to provide accurate diagnostic information. It often falls on physicians to ensure patients understand the importance of the tools and maintain consistent use. The “digital divide” may block some patients from using these tools altogether; as many patients can’t use technology due to lack of resources, low digital literacy, language barriers, or cognitive impairment.
Balancing technology with clinical skills
While not reflected in the polling data, Sermo members’ comments reveal concerns about maintaining fundamental clinical skills alongside technological adoption. Multiple physicians emphasized the importance of preserving traditional diagnostic approaches and clinical judgment.
“The new technologies are great – but too many people depend on them to answer their questions and are losing or don’t have major clinical diagnostic skills,” expresses a family medicine physician.
Another family medicine physician shares the same sentiment: “Although I like having the backup of quality technology, I find that many of my newer colleagues have substituted good clinical acumen with technology. This is not only sad but dangerous.”
A GP argues for the importance of traditional approaches. “I’m quite old school and not so well versed in the newest technologies,” they write. “Good old diagnostic tools like asking relevant questions, listening to the patient and doing a regular thorough physical examination takes you pretty far.”

Adopting and interpreting new diagnostic technologies with confidence
Physicians on Sermo have shared their experiences with adopting newer tools. They don’t all implement new technology with the same level of urgency. In the Sermo poll, 14% of physicians reported “always” adopting new technologies immediately upon availability, while 55% said they “often” embrace them. 21% of physicians adopt new technologies “sometimes after seeing peer adoption.”
For those who are more hesitant, a lack of confidence may be at play; only 16% of physicians reported feeling “very confident” in interpreting results from genetic panels, molecular assays and other advanced diagnostic tools. 40% said they only feel somewhat confident.
But, Sermo members who have adopted new tools have reported positive experiences. “As a Radiologist I use advanced imaging on a daily basis in my practice,” one member writes. “But what I believe has really transformed diagnostic imaging in recent years has been the advent of molecular imaging, especially in regards to PET scanning and the use of novel radiopharmaceuticals to both diagnose as well as treat cancers (Nuclear Medicine Theragnostics).”
A nephrologist and Sermo member shares a similar remark. “There has been significant progress in diagnostic imaging technology,” they write. “I notice this in my daily practice, and this has helped me significantly in establishing certain definitive diagnoses.”
Navigating the future of medical diagnostics
Diagnostic technology continues to reshape medicine. Feedback from Sermo members indicates that these innovations are making positive impacts across medical specialties.
The Sermo community has a measured approach to technology adoption, with a majority often embracing new tools after careful evaluation. Even those who are excited to adopt new technology may face challenges, from cost and insurance coverage limitations to lack of patient compliance.
Physicians navigating this evolving landscape can connect with peers who share similar challenges. The Sermo community offers a collaborative environment, where more than 1.5 million healthcare professionals across 150 countries share insights and advice based on their own lived experiences. Whether you’re exploring new diagnostic technologies, seeking interpretation guidance, or sharing your experiences with innovative tools, you can engage with your professional community to accelerate your learning.