42% of physicians on Sermo say they’ve seen at least a slight increase in drug resistant fungi infections like Candida auris or Aspergillus in the past 12 months, according to a recent community poll.
While that figure doesn’t represent a majority, it signals a noticeable shift, particularly in high-acuity and immunocompromised settings. Yet, this trend isn’t universal.
As one general practitioner within the Sermo poll comments noted, “I haven’t seen an increase in fungal infections, but maybe in other places with more tropical weather or rural areas.” That raises a broader question: what’s driving this uneven rise and how are physicians responding to what many describe as a slow-burning clinical threat?
This article explores that question using a combination of poll data and comments from the Sermo physician community. What emerges is a picture of differences in adapting to the new threats posed by drug resistant fungi, concern among physicians about the level of preparedness and growing awareness of systemic vulnerabilities in the face of drug resistant fungus.
The impact on clinical practice for physicians
When asked about their biggest concern regarding drug-resistant fungal infections, 39% of Sermo respondents pointed to limited antifungal treatment options.
As one general surgeon on Sermo put it, “There has been a rise in the incidence of fungal infections. My main concern is the lack of adequate antifungal drugs.” That concern extends beyond access and challenges whether the necessary drugs even exist to tackle the problem. However, simply getting new medications isn’t enough—physicians are also wary of the toxicity profiles of new treatments, especially in vulnerable populations. Another GP warned, “Sometimes the benefit is diminished by the damage caused by the antifungal drug.” It’s a reminder that any innovations must be clinically realistic and thoroughly tested, not just novel.
Another 22% cited increased morbidity in immunocompromised patients as their top concern. These include transplant recipients, patients undergoing chemotherapy, those living with HIV and individuals recovering from sepsis or major surgery. Mortality associated with drug-resistant fungal infections rates in immunocompromised patients can reach up to 90%. “Invasive fungal infections with resistant pathogens are on the rise, especially in immunocompromised patients,” wrote one Pulmonologist on Sermo.
However, the concern isn’t evenly distributed. A cardiologist admitted, “Not something I regularly deal with in my practice,” highlighting how siloed specialties can be in their experience of emerging threats. Still, there’s a growing consensus that while the most vulnerable may be impacted first, resistant fungal infections could eventually touch broader clinical contexts.
13% of respondents highlighted the lack of rapid diagnostic tools. Conditions like Candida Auris, a drug-resistant fungus, can be difficult to identify quickly, leading to critical treatment delays. One pediatrician pointed out, “[Drug resistant fungus] Candida auris, for instance, poses serious challenges due to both resistance and identification delays. We need more proactive surveillance, faster diagnostic tools, and updated protocols.” It seems there’s a concern that public health systems need to quickly catch up to foreseen spikes in demand.
Other concerns included inadequate public health surveillance (11%), overlap with bacterial co-infections (8%) and low institutional preparedness (5%). Physicians in public systems noted they often lacked even the most basic tools for fungal identification, pointing to under-resourced infrastructures. “Doctors who work in public institutions in Mexico are unable to diagnose infections due to a lack of resources,” said one pediatrician. Another radiologist took a broader view, saying: “Yet another burgeoning issue as we dismantle public health here in the US.”
These perspectives suggest that, beyond diagnostics and drugs, combating fungal resistance will require renewed investment in public health infrastructure, both physical and political.
What’s driving fungal resistance? Climate and other factors
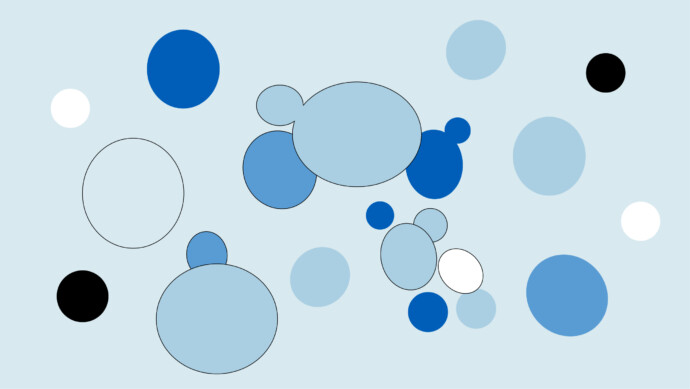
In the same Sermo poll, physicians were asked: “To what extent is climate change influencing the spread of drug-resistant fungal pathogens?” The answers were mixed.
- 19% saw it as a major contributing factor
- 33% said moderate
- 24% called it minor
- 10% rejected the idea entirely
- 13% weren’t sure
Those who viewed climate as a major factor linked it directly to real-world changes in their practice. One GP observed, “Climate change is a growing public health concern. Not only does it have an environmental impact, but it also has direct clinical repercussions, including increased resistance among fungi and other pathogens.” As a more specific example from a physician on Sermo living in El Paso, Texas, rising dust storms are blamed for surging cases of Valley Fever, with one internist writing, “Climate change is the underlying factor.”
But there is disagreement when it comes to the topic of climate. One family physician dismissed, “I don’t think climate change has anything to do with it. Period.” This suggests that, while environmental shifts are clearly influencing disease patterns in some areas, strong skepticism on this idea remains – perhaps driven by how it’s framed politically, personal knowledge gaps, personal ideologies, or even evidence specific to a physician’s region of practice.
Aside from climate, this study (2024) identified a suite of causes driving fungal resistance. Most important among them is the widespread use of immunosuppressants. Medications like corticosteroids and azathioprine are known to suppress immune function, leaving patients more vulnerable to infections. This is a point raised by several Sermo members, with one family physician arguing, “Fungal infections, often opportunistic, are present in immunocompromised patients under prolonged treatment with immunosuppressants. Early detection is essential.”
There’s also growing concern about the overuse of broad-spectrum immunomodulators. As two GPs put it, “Drug resistance: antibiotics, antifungals… are, unfortunately, increasing! The problem is serious!” and “Resistance to the use of antifungals appears all over the world, making the indiscriminate use of antibiotics increasingly dangerous.” These comments echo the warning that overreliance on immunosuppressive drugs may be fuelling the very infections they leave patients vulnerable to.
And while not a central focus of the aforementioned paper, environmental exposure to agricultural fungicides also came up. One GP said, “Dangerous fungal infections… are evolving resistance to the drugs meant to fight them. Scientists believe such mutations arise when fungi are exposed to agricultural fungicides.”
Ultimately, the resistance crisis is being shaped as much by what happens in fields and farms as it is in hospitals.
Physician strategies for managing drug-resistant fungal infections
In terms of how physicians are adapting to changing fungal threats, the response has been cautious and nuanced:
- Only 21% of Sermo respondents said they’d adjusted empiric antifungal therapy based on local resistance patterns
- 19% have increased diagnostic testing for at-risk patients
- 17% have increased their use of infectious disease consults
- 11% have participated in continuing education about this subject
- 13% reported updating infection control protocols
- 14% have made no changes at all.
Several physician comments shed light on their reasons for making changes to their working practices. A GP noted, “I now more frequently integrate rapid molecular diagnostic tests and more targeted antifungal regimens based on local resistance profiles. Coordination with microbiology has become key.”
Other physicians are taking the approach that this is a problem more for politicians than physicians. One pediatrist said, “I believe that hygiene and public health policies are important and that governments should give priority to this issue; unfortunately, they seem to be going in other directions.” This suggests that physicians can do only as much as the resources and political environment will allow, and that to do more may require a top-down approach from world governments.
Indeed, not everyone is changing course. A gynecologist admitted, “So far I haven’t seen changes, but I will be more aware. We may start new protocols if this keeps escalating.” And a cardiologist added, “Not something I regularly deal with in my practice. Of course, effective means for addressing this are needed.”
These comments highlight a key point that for many physicians, fungal resistance remains a concern to keep their eyes on. Physicians should prioritize strategies such as rapid, accurate fungal diagnosis and susceptibility testing to tailor antifungal therapy, use combination or new agents when needed, practice antifungal stewardship to avoid overuse, enforce strict infection control to prevent spread, collaborate across specialties, and educate patients for adherence—all to effectively manage drug-resistant fungal infections.
What support are physicians looking for?
While 49% of respondents said they felt at least somewhat confident in diagnosing fungal infections in immunocompromised patients, 25% reported feeling somewhat or very unconfident. This confidence-action gap is worth interrogating. Clinical awareness appears to be outpacing systemic preparedness. Even where concern is high, practice changes remain scattered and piecemeal.
As one GP commented, “This just emphasizes the burning need for more research into mechanisms of drug resistance in fungi and the development of new therapies.” Others called for access to better diagnostics, faster molecular tools, and clearer treatment protocols. A reproductive endocrinologist noted, “The very fact that these infections are not common increases the risk there can be delays in diagnosis.”
Some physicians place the onus on system-level change. “Strengthening infection control and lab capacity is no longer optional,” wrote one pulmonologist. Others work in settings where preparedness is already high. “I am thankful to live and work in an area that keeps up with the latest guidelines and is well plugged in with infectious disease specialists,” said a family medicine doctor.
What’s clear is that the global clinical landscape is deeply uneven. While some health systems are proactively adapting, others remain stalled, either due to resource constraints, clinical silos, or skepticism. Leading authorities like WHO emphasize that fungal diagnostics remain a critical gap in many health systems, especially in low- and middle-income countries where complex tests are unavailable, leading to delayed or missed diagnoses and ineffective treatment. This disparity amplifies challenges in managing antifungal resistance globally.
The rise of drug-resistant fungi may be slow and regionally variable, but physicians across the board are beginning to see the contours of a new challenge. Whether the support they need arrives in time remains the bigger question.
Your takeaway
Antifungal drug resistance in Aspergillus and Candida Auris aren’t yet a universal crisis, but they’re a growing clinical concern as physicians increasingly see rising infections, limited treatment options and uneven preparedness.
While some are adapting with new protocols and diagnostics, others remain hesitant or unsupported. The challenge is layered: medical, environmental, systemic and not confined to one sector, with even areas like farming playing their part.
What comes next depends on how quickly healthcare systems can close the gap between emerging threats and the tools needed to fight them.
Join the discussion on Sermo
How are you coping with the rise in drug-resistant fungi in your practice?
Share your strategies, see how peers are navigating these challenges, and get involved in real-time discussions about what works.