In a healthcare practice, effective communication is very important and a lot of healthcare organizations are becoming more aware of the need to improve communication. Effective communication between healthcare professionals is particularly essential for effective operations, patient safety and quality healthcare delivery. However, achieving this seems rather difficult in some healthcare organizations. Effective communication is often stymied by certain challenges.
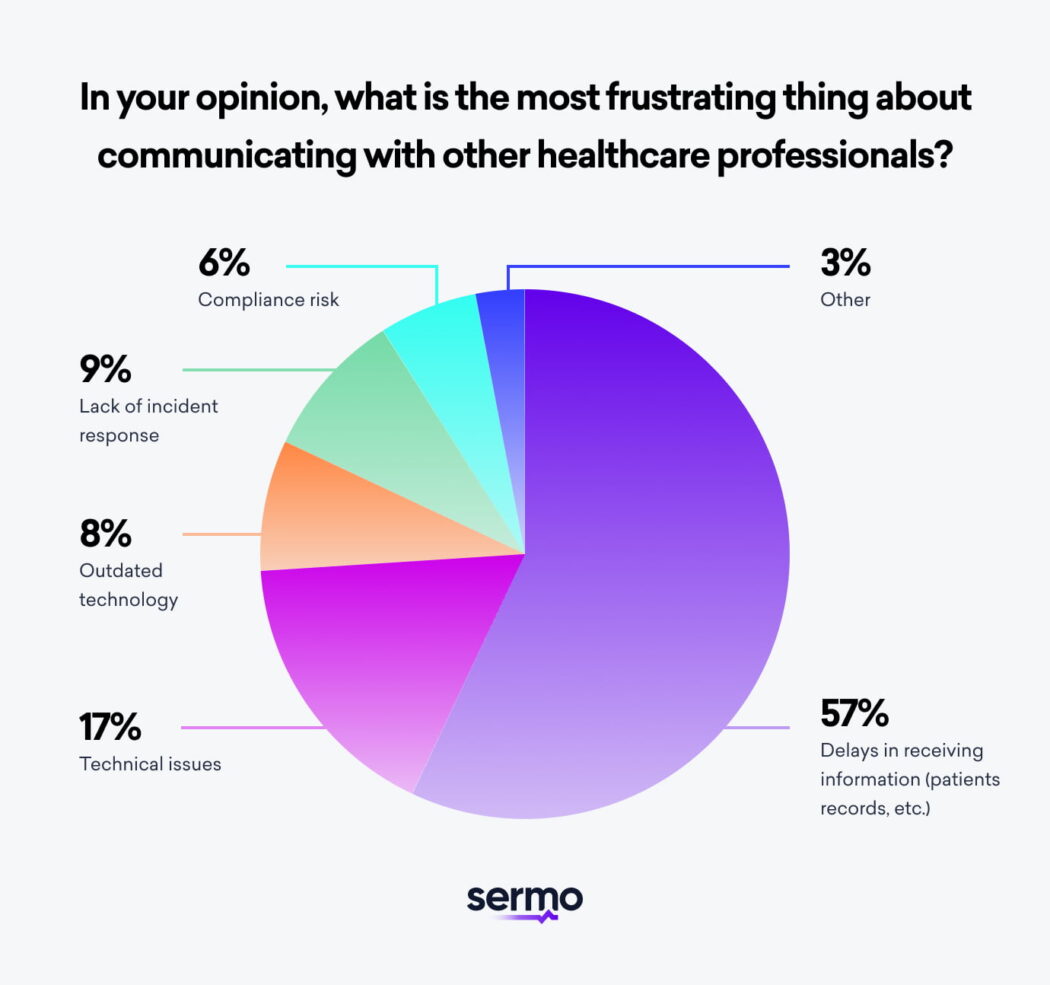
We asked physicians in a recent Sermo poll about some of the obstacles to effective communication. Delays in receiving information, technical issues, lack of incident response and outdated technology were the most common challenges.
Perhaps you too are struggling with these challenges and wondering how to improve communication with other healthcare professionals? This article dives deeper into the importance of effective communication in the healthcare setting, the types of healthcare communication and tips for effective communication.

Why effective communication is important in healthcare
The healthcare setting is a dynamic environment with various healthcare professionals, diverse healthcare teams and multiple clinical data collected from both in-patients and ambulatory patients. Patient information has to be shared amongst healthcare professionals in a clear, effective and timely manner in order to devise an appropriate care plan and prevent adverse or fatal events.
Sometimes, physicians have to share patient information with other physicians in different healthcare facilities. A Sermo poll reports that 68% of physicians communicate with other physicians at least once a week. Communicating with other physicians is also important to enrich patients’ health.
Here are some of the reasons why communication is important in the healthcare field.
1. Patient safety
Patient safety remains the utmost reason for effective communication in healthcare. According to a Sermo poll, 63% of patients consider patient safety as the most important topic in effective communication in healthcare.
Multiple studies and narrative reviews suggest that poor communication in any chain of communication in healthcare can result in poor comprehension, medication errors and poor patient compliance which can all risk a patient’s safety. According to The Joint Commission more than 60% of all hospital adverse events they reviewed has been linked to poor communication1. Studies have also demonstrated that poor provider-provider communication can lead to surgical complications or death2.
An effective communication strategy that characterizes transparency, clarity, accuracy and urgency can significantly improve patients’ safety. Such strategies are increasingly important in high risk units such as the intensive care unit and the emergency department.
2. Improved decision making
Without a doubt, physicians and health care professionals can make better decisions when they are well-informed. Decision-making is a shared responsibility between patients and physicians and comprehension is important for the best decisions to be made.
For physicians and other healthcare professionals, clinical data should be shared seamlessly between all relevant teams accurately, clearly and timely. Being able to devise an appropriate care plan is dependent on this. Effective collaboration and strong communication between healthcare professionals and providers can also improve awareness of each person’s or unit’s understanding3 and increase confidence in decisions made4.
3. Improved job satisfaction
Communicating well with colleagues is certainly an essential caveat of successful team collaboration. Effective communication between healthcare professionals can help foster teamwork, boost confidence in decisions and improve working relationships.
Studies have shown that communication between healthcare workers is a major contributing factor to clinical effectiveness and job satisfaction5. Poor communication about responsibilities and other inappropriate behaviors have been observed to negatively affect staff relationships, job satisfaction and turnover6. A cohesive healthcare team requires effective communication characterized by trust, mutual respect, transparency and collaboration. This encourages teamwork and promotes continuity and clarity within the patient care team.
4. Improved patient satisfaction
Effective communication between healthcare professionals can have a ripple effect on patient satisfaction. Poor communication between team members can reflect on interactions with the patient and their family. Due to poor communications, patients who are the consumers of healthcare services may receive conflicting information or incomplete information that leave them confused. This may lead to tragic consequences and healthcare professionals must understand that in this case, the patient is the victim.
There is evidence that shows that poor communication in healthcare can lead to not only patient dissatisfaction but also discontinuity of care7. Improved information flow and good communication can significantly improve patient satisfaction.
“Effective communication in healthcare provides good relationships and good team work and these help to improve patient satisfaction.”
Sermo, Pediatrician

Types of communication in healthcare
Communication in healthcare makes a difference every day. Physicians communicate with other healthcare professions within the hospital and with other providers at other hospitals. Even outside of the healthcare institution, physicians communicate with each other both formally and informally.
Intrahospital communication vs Interhospital communication
Intrahospital communication involves sharing information within the same hospital or healthcare facility. Besides the patient’s clinical data, other important information such as scheduled appointments, requested tests, room changes and scheduled surgeries need to be shared effectively and seamlessly with relevant stakeholders in the care management chain.
Interhospital communication on the other hand involves sharing patient’s clinical data with other hospitals. This is mostly necessitated when a patient is being transferred to another hospital for further treatments or other reasons.
Communication methods
Just like there are different communication methods we use in our day-to-day lives, there are different communication channels used in healthcare. In recent times we have seen a remarkable rise in the use of digital tools and cloud communication platforms in the healthcare field by physicians, nurses, diagnostic technicians, and other medical personnel to improve efficiency and quality in healthcare delivery.
Healthcare professionals should know how to use the different communication methods and when to use each method. Misuse or abuse of a communication method can have serious consequences on patient safety. Hence, healthcare organizations should prioritize training its staff on the various communication channels used to share information.

Here are some of the common communication methods used in healthcare facilities.
- Sharing patient data externally
Patient records are very crucial and also sensitive. They are often shared within the hospital and with other providers. Patient data can include sensitive patient information including names, birthdates, health conditions and treatments and these should be shared securely.
Several digital tools are available for sharing patient data but it is important for healthcare organizations to use HIPAA (Health Insurance Portability and Accountability) communication tools to ensure patient data is shared securely. The HIPAA security rule requires that patient data should be encrypted whenever possible. Digital platforms like Accellion, Dropbox and OneDrive are HIPAA-compliant systems that are used to share patient files externally.
It is also important that patient data is transmitted in a timely manner. Delays in receiving patient information can jeopardize patients’ safety and can cost hospitals millions of dollars each year in unnecessary expenses.
- Online patient databases
Thanks to digital tools and cloud-based databases, healthcare professionals can access patient data, share information and collaborate better on patient care. In a recent Sermo poll, 34% of physicians indicated they used Centralized data systems (transmitting patient data, sending secure messages, etc.) as their primary method of communication with other healthcare professionals.
It is required that these platforms are HIPAA-compliant for safe and reliable exchange of information.
- Use of automated mail/notification systems
With Automated systems, healthcare organizations can send out certain information automatically. They can also be used to send out information broadly for instance to the whole department or to the entire hospital. Information that can be sent out with such systems include schedule changes, new staff joining the hospital, emergencies and general hospital information. When used with RFID tags, these systems can be used to track patients in wards where this may be needed (e.g psychiatric ward) and also to track medical equipment.
Healthcare organizations can also use such platforms for sharing certain information with their patients. Automated notifications systems help to minimize errors in healthcare communication and also save time.
- Communicating on professional social networks like Sermo
Professional social networks are also an excellent way to collaborate with other healthcare professionals. The “informal” avenue it provides allows borderless collaborations and educative conversations with a wider group of medical professionals.
Sermo is a platform for physicians that offers a unique physician-first online community that allows clinicians to communicate about issues that are important to them and their patients.

Tips for effective communication between healthcare professionals
1. Define communication methods and train staff
As earlier mentioned, there are quite a number of communication channels and each has its advantages. For efficient communication, healthcare organizations should define the methods that work best for them and also define how and when each should be used.
For instance, in the event of emergencies, emails may be ineffective and if used may have serious consequences. Healthcare organizations should define how these methods should be used and train all staff as well on this.
Cloud-based platforms and centralized data systems can be a bit complex but are an excellent tool for sharing medical records across teams. Medical personnel and administrative staff should be trained on how to use these tools in order to optimize them for patient safety and patient satisfaction.
2. Promote communication as an organizational culture
If communication and transparency are key essentials of the organizational culture, the work is half way done. Healthcare organizations should deliberately inculcate communication in their structure, operations and practices. This way it is easily normalized and staff can uphold it.
This also helps in building effective and successful teams, improves work relationships and increases job satisfaction.
3. Create systems for collaboration
Creating opportunities for physicians and other healthcare professionals to collaborate can improve effective healthcare communication. Whether formal or informal, these interactions can influence patient safety and improve quality of healthcare. Open conversations, team briefings and collaborative ward rounds are some of the opportunities that can foster collaboration and communication.
A major barrier to collaborative interactions of interdisciplinary units in the hospital can be the hierarchies. Studies show that hierarchical differences, role conflicts, worries about upward conflicts and the complex network of relationships can impair effective communication in healthcare organizations8. It is common to find medical personnels of lower hierarchy a bit restrictive or uncomfortable to voice out their concerns or even share their ideas. In the case where the physician at the higher end of the hierarchy is intimidating, it is safe to conclude that communication is distorted and less collaborative.
Fishing out these issues is important and the healthcare organization should identify ways to promote interdisciplinary collaboration free of any disruptive behaviors.

4. Review and assess the communication system and policies periodically
For continuous quality improvement of communication in the healthcare setting, there is a need to assess the current system and policies in place and upgrade and adjust if needed. Healthcare teams should have the overarching goal in mind and continuously improve the methods and systems of communication.
Periodic patient and staff surveys are an excellent way to get feedback on the communication efficiency and satisfaction of patients. The responses from such surveys will spark valuable insights and will help improve the current communication system in the healthcare facility. Other things healthcare organizations should assess is disruptive behaviors that can negatively affect communication and its cause.
5. Use digital tools and other interventions
In today’s world, technology makes things easier and faster. Using digital tools and other technology interventions that comply with HIPAA rules for healthcare communication is forward-thinking. Digital communication tools can help faster communication and collaboration with other medical professionals.
A centralized data system that keeps all clinical data and medical records in one database but makes it accessible to many has numerous benefits. These data systems help to improve data integrity and accessibility, reduce costs, save time and facilitate real-time collaboration with interdisciplinary teams.
Other digital tools include HIPAA-compliant texting apps such as Medchat, TigerConnect and Curogram for encrypted 2-way messaging and mail systems like Post Grid for automated emails and notifications.
By introducing these technologies in healthcare operations, care coordination is more straightforward and better organized.
6. Join a professional social network
Professional social networks are excellent informal platforms for collaborating with other medical professionals. On such networks, medical professionals can express themselves freely about their concerns, join interesting conversations and learn about research findings from other colleagues. Social media platforms like Linkedin and Twitter are great for meeting other professionals and joining conversations. While these social networking sites can be very helpful to physicians and patients alike, platforms specifically targeted towards physicians can be even more beneficial.
On physician-targeted networking platforms, physicians can connect with numerous medical professionals and ask other medical professionals about career advice, share and learn from each other’s experiences. In addition, they can seek medical advice from other physicians about their own patients and have a more in-depth conversation. The benefits are endless.
The importance of communication between healthcare professionals can not be over emphasized. It however remains a common challenge to most healthcare organizations. It can be rather complex to surmount but it is definitely achievable. When done right, it can significantly improve patient safety, patient satisfaction and staff satisfaction. The importance of communication between healthcare professionals is a developing conversation in the Sermo community of physicians.
To follow the conversation and learn more about ways to improve communication in healthcare and get access to paid physician surveys, sign up to Sermo today.