The doctor-patient relationship is complex, unique and multi-faceted, and it is only evolving more with time. As time and compensation becomes tighter for physicians, the danger is that patient interactions become distant and clinical in order to make room for more appointments per day. Many doctors find themselves rushing to take on extra work for additional compensation, sacrificing their ability to build rapport with existing patients. In fact, when polled, 43% of Sermo physicians said that they had insufficient time to build relationships with their patients. For many, gone are the days when one doctor can care for one family throughout the generations, and be a constant source of reassurance.
What does the doctor-patient relationship mean in 2022?
There are, of course, certain pillars of this relationship that should be consistent and unbroken. Namely: benevolence, trust, and confidentiality. At the core of what physicians do is to have the patient’s best interests at heart; to heal, and to improve their quality of life, above all else.
Benevolence and confidentiality go hand in hand – to keep your patients’ information secure and confidential, and to abide by the laws governing this part of medical practice. With both of these, comes trust. 27% of Sermo physicians polled said that trust was the most important part of the doctor-patient relationship, and it’s clear why. Without confidentiality, without care and compassion, there can be no trust. If a patient cannot trust that they are being cared for in the best way possible, much of the relationship falls apart.
27% of Sermo physicians polled said that trust was the most important part of the doctor-patient relationship, and it’s clear why.
What about the technical aspects of the relationship? For many patients, it is as important that their doctor be competent and confident in examination, diagnostics, prognostics and intervention, as it is that they trust their physician and feel cared for. Are you able to provide not just adequate care in these arenas, but also practice evidence-based medicine, consistently seeking new information from the literature and peers as needed?
One facet of this relationship continues to evolve throughout history – the importance of compassionate care in addition to competent care. A kind “bedside manner”, stands today to be an incredibly important key in developing the doctor-patient relationship. 45% of Sermo physicians polled stated that communication is the most important part of the doctor-patient relationship. Communication, professionalism and creative patient education techniques are now a core part of medical education, emphasized as fully as technical skills. Medical schools now understand the necessity of producing doctors that are able to communicate information in a way that best assists each individual patient – without judgment – despite socio-economic, cultural, or cognitive barriers.

Why is the doctor-patient relationship important?
When polled, Sermo members listed trust, communication, physician empathy, and professional boundaries as important components of the doctor-patient relationship. Why, though, is it important to build this relationship?
A successful dynamic between patients and their physician not only improves the outcomes for a doctor and patients, but for healthcare as a whole, and for generations of physicians and patients to come.
With effective communication, patients become empowered to advocate for themselves; to understand their own conditions and become collaborative in decision-making with their doctor. They are no longer passive in the experience, but can often provide valuable insight into their condition that will allow for better intervention on the part of the physician. Similarly, by avoiding miscommunication, doctors have more control over their patients’ actions outside of the medical office. With a greater understanding of their options, and of the importance of compliance with their plan of care, patients may improve the efficacy of their treatment, and it is important for their physician to implement this.
As mentioned previously, trust is a vital part of the doctor-patient relationship. Trust, whether as a result of successful patient outcomes or physician competence, or simply by usage of more effective communication skills and compassion for the individual, may also encourage greater compliance to a given plan of care. Overall, patients who are more satisfied with their plan of care – and more trustworthy of the physician delivering it – will have better outcomes, and will be more likely to continue with their current provider (1). This provides both convenience for the individual, and improved financial possibilities for the provider’s location.
How can the patient-provider relationship improve healthcare as a whole? For many patients, trust in a provider is not just trust in that individual, but in the profession as a broader entity. As healthcare continues to focus on developing into a more patient and family-centered model, it is imperative that physicians encourage collaboration, understanding, and reassurance in their relationships with patients, in order to nurture this progression for healthcare providers and their industry.

Keys to a successful doctor-patient relationship
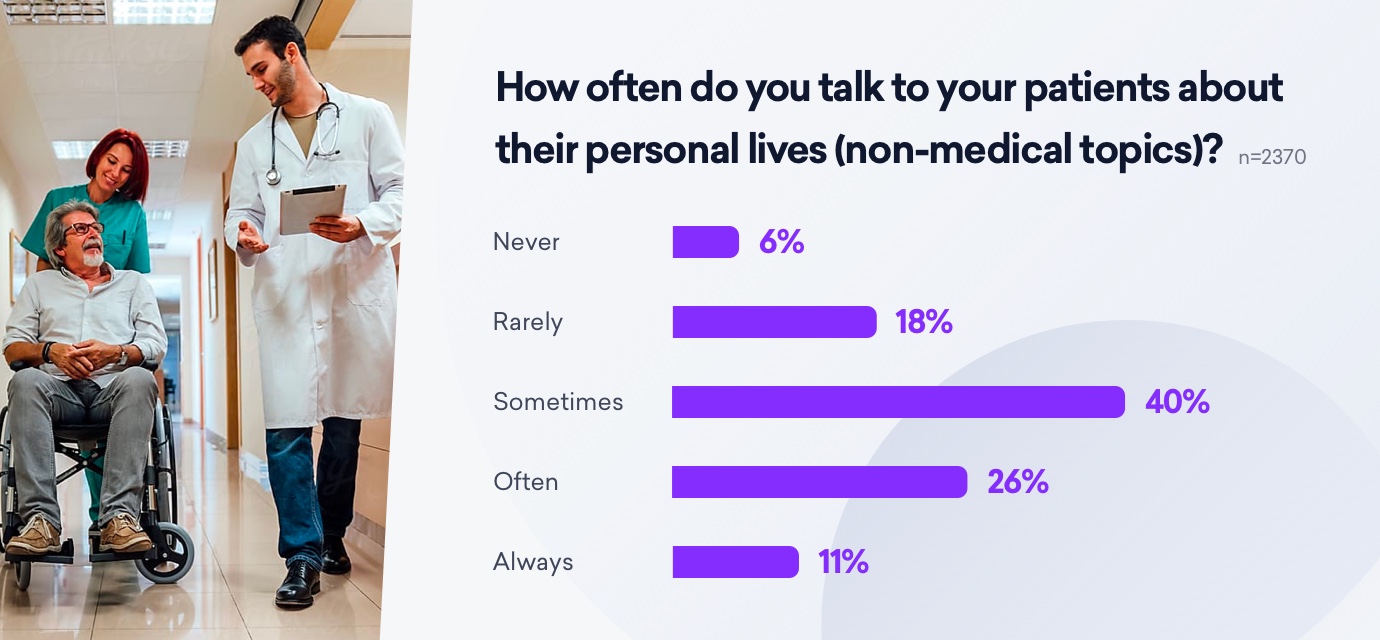
When polled, only 11% of Sermo physicians stated that they “always” talk to their patients about their personal lives or personal matters. When asked why this was, some stated concerns about breaching professional boundaries, making patients uncomfortable, or fears that a doctor talking to patients about their personal issues would be seen as “meddling” in their lives.
However, as we know, the physical condition of patients does not exist independent of the emotional one. There are a multitude of impacts on a patient’s life that may significantly alter their compliance to a plan of care, their understanding of their condition or their response to treatment. By developing open lines of communication about a patient’s personal lives – to an appropriate extent – physicians may be able to care for their patients in a more holistic and effective way.
Sermo physicians listed several barriers to communicating openly with their patients; most commonly, time. Several physicians surveyed stated that unless in private practice, there was simply not enough time for them to administer appointments that were financially responsible and encompassed everything they wanted to talk about with their patients.
With pressure to address the physical concerns, 43% of physicians stated that they did not have time to develop good relationships with their patients. For the remaining 57%, however, there were ways to build empathetic communication into their session – some suggestions were to develop more critical active listening skills, so that they may pick up on things patients share during routine examinations and history taking. From here, it was suggested that patients would be more likely to trust a physician who could identify personal areas in which they were struggling.

Another important point that Sermo physicians raised was one of informed consent. Many physicians stated that in order for a successful doctor-patient relationship, it was imperative that patients do not feel judged. This includes not just obtaining informed consent at each step of the examination and treatment, but respecting the boundaries of the patient. Sermo physicians suggested that patients needed to understand all options and alternatives available to them before treatment was administered, and in doing so, physicians would be able to build a stronger physician patient relationship.
To obtain and maintain professional boundaries with patients – only 4% of Sermo physicians claimed this to be the most important part of the doctor-patient relationship – it was stated that there is a fine line between presenting a professional and competent front, and narrowing the gap between patient and doctor. Sermo physicians suggested that while some patients may respond to an authoritative approach, with the doctor taking charge of each interaction and leading the plan of care, patients also needed to feel heard and seen, and that they should be taken seriously in their concerns and allowed sufficient input into their treatment.
How does your clinic measure the success of your doctor-patient relationships? A huge 79% of Sermo physicians stated that the best way to measure how well doctors and patients were working together was in-person, during the appointment. Despite the prevalence of surveys and questionnaires, often forgotten in patient inboxes or ignored at patient outtake, only 18% thought they were effective ways of truly gauging how happy patients were with the relationships formed with their physician. Physicians should be open with asking patients about their happiness, and how they can better improve, and Sermo physicians suggested that this can be done face-to-face during treatment. When asked, several Sermo physicians saw this as an essential part of patient care evolution and professional growth for the provider.
Models for patient-provider relationships
There are currently four common models for approaching the doctor-patient relationship.

The Paternalistic approach encompasses much of what has been discussed above – a patient provider relationship in which the doctor takes charge of the conversation, and forms opinions about their patients’ care with no input from the patient. In this model, the physician uses their knowledge base and experience to “guard” the patient, and care for them as the doctor best sees fit. While perhaps the most traditional model of patient-provider care, and one that many patients still expect and occasionally fear, it is considered that this model is best employed either in emergency situations, or when the patient is not able to advocate safely for their condition. In this model, the physician independently promotes the best treatment option for the patient without collaboration or even consent.
On the other hand, the Informative model of patient care, or consumer model, allows the physician to exercise their expertise by providing all the technical information necessary to define a patient’s condition and inform the patient of all interventions available. Most importantly, in this model, the patient is the one to select their treatment based on the information provided by their physician. Ultimately, the patient is in charge. It is therefore imperative that the physician provide the patient with both information and unbiased opinion on the best next steps. In patient–centered locations, this is considered to be the best model for doctor and patient.
The Interpretive model is one in which the physician plays “advisor”, selecting the most appropriate method of treatment as determined by them, and administering it with the patient’s consent. This is the model many patients are used to receiving and is used where time-saving is a concern.
Finally, the Deliberative model is one in which the physician is not only a medical provider to the patient, but a friend. The doctor informs the patient of the best treatment for them, and encourages and assuages their concerns at each step of the way. They ensure the patient understands the value of the medical measures being taken for them, and teach them about their condition and their expected outcomes. Patient consent is also necessary in this model (2).
It could be argued that any one of these models for patient-provider care may be appropriate given the setting or situation. It could also be possible that some combination of all models, or taking certain elements from each, could create a singular model in which the doctor-patient relationship is centered, and most likely to succeed.
For example, a physician can offer all technical and factual information to a patient about their condition, carefully delivering the information in a way that is both impactful and sensitive, helping them truly understand their condition and any tests and measures completed during their examination or plan of care. They then might be able to advise on the selection of one treatment over another, despite always informing each patient about every risk, benefit, and alternative to a treatment modality. Because this patient is truly informed, and collaborative in their care – the choice is theirs in the end – this may improve trust between the doctor and patient, and open lines of communication to more effectively move forward the patient’s plan of care. Finally, despite all of the above, the physician stands to deliver emergency treatment that may deviate from a previously-decided plan, should not doing so harm the patient.
Improving your patient-provider relationships with networking
How do you develop your own model as a physician for an effective doctor-patient relationship? Collaboration with other physicians may give you the insight you need – to learn successful tactics, to better improve your own skill set, and to elevate your practice and career. Real Sermo physicians came together to discuss how they have developed the best patient-provider relationships possible.
If you’re struggling to find common ground with your patients, or find yourself losing patients to other providers due to your relationships, it might be time to reach out to other providers for assistance. Social networks like Sermo are built just for you – they allow verified physicians from all over the globe to come together and share their expertise.
At Sermo, you always have a friend and a peer, just a click away. Already an expert at patient-centered care? You can help others build their patient-provider relationships today, all by commenting and contributing on questions posted by real doctors. If you feel isolated by typical social networks, and wish you could interact with others who truly understand your profession and the challenges you face, signing up for a free Sermo account is all you need to get started towards improving your patient-provider relationships.
Click here to sign up today, and be the best provider you can be.
References
- Lee, S. J., Back, A. L., Block, S. D., & Stewart, S. K. 1 January 2002. Enhancing physician-patient communication. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/12446437
- Smith, Yolanda. “Doctor–Patient Relationship.” News, 20 June 2019, https://www.news-medical.net/health/DoctorPatient-Relationship.aspx