According to a recent Sermo poll, 56% of physicians believe that pre-procedure coaching sessions could be used within their medical practice. Yet, 28% remain unsure whether the benefits would outweigh the challenges of implementation.1
So why do some doctors remain hesitant? And what further assurances and resources do they need to embrace coaching more fully within their medical practice?
This article uses Sermo survey data and direct quotes from our community of global physicians to explore the evolving role of medical coaching in modern healthcare, its tangible value, and the barriers still holding it back.
What is physician pre-procedure coaching and why does it matter?
Pre-procedure coaching, also known as just-in-time (JIT) training, involves providing physicians with short, targeted training on specific procedures. It’s usually given just before they carry out particularly high-risk or rarely performed surgeries.2
Unlike traditional training or doctor mentorship programs, which focus on long-term education on general improvement, JIT is short-term and focuses on a specific task at hand. It’s focused, timely and depends on the situation to give physicians immediate support only where they most need it.
The need for JIT is motivated by many physicians having a lack of experience and exposure to specific procedures. In these scenarios, 80% of physicians in this Sermo poll said that infrequent practice impacts their confidence or performance:
- 28% said it affected them frequently
- 52% said occasionally1
Indeed, pre-procedure coaching gives physicians an immediate confidence boost within high-stakes situations. The results speak for themselves:
- Higher first-attempt success rates: One example study within pediatrics showed that inexperienced clinicians who received coaching before infant intubation saw a 91.4% first-attempt success rate, compared to 81.6% without coaching. Similarly, resident physicians improved from 81.4% to 93% with pre-procedure training.3
- Reduced mental strain for fewer errors: JIT coaching has been shown to alleviate the mental burden during stressful procedures. 2 Research in the Journal of Surgical Education found that coaching programs for surgeons can reduce workplace stress and burnout, validating the psychological and performance-related benefits of JIT coaching.
Additionally, this controlled trial on junior surgical residents demonstrates that just‑in‑time reflection and coaching—delivered immediately after one crisis and before the next—can prime clinicians cognitively and reduce their workload when facing another high-stakes surgical scenario.
- More efficient working practices: Coaching sessions as brief as 10 minutes can be integrated into practice without causing delays.2 For example, microlearning formats, such as videos or tip sheets, have been shown to be in demand by 93% of physicians in a recent survey.5
During quick process changes, like health crises or new COVID-19 procedures, JIT simulation helps clinicians quickly learn and adapt without the delays of traditional training. For instance, one study demonstrated 95% compliance with new workflows following targeted JIT training, along with lower staff infection rates, indicating behavioral change and increased readiness.
- Saving costs: Education before operating has also been shown to cut ICU stays and hospitalizations, which can ease the burden in the broader healthcare system.6
Just-in-time (JIT) coaching significantly reduces healthcare costs by decreasing error rates and minimizing the need for formal retraining. It optimizes resource utilization and prevents burnout, retaining skilled staff and facilitating faster adoption of new protocols. These benefits lead to fewer complications, improved efficiency, and substantial savings for healthcare organizations.
While pre-procedure JIT doesn’t replace the value of long-term experience or mentorship, it complements both by offering timely reinforcement when it matters most.
What types of coaching do physicians find most valuable?
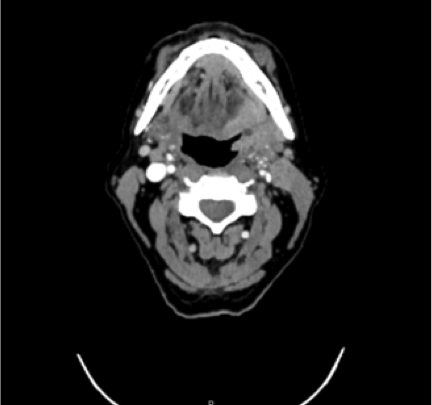
According to a Sermo poll, 45% of physicians agree that pre-procedure coaching is most valuable for high-risk, low-frequency procedures, such as pediatric intubations or rare surgeries.1 These are often the procedures where clinicians feel the most pressure to perform perfectly yet don’t have the benefit of regular practice.
- 22% of physicians believe routine procedures could benefit from coaching, emphasizing its role in building confidence, ensuring quality, and reinforcing best practices.1 This need reflects both technical support and the desire for emotional reassurance and professional accountability.
- Emergency interventions (20%) are also valued for coaching, as timely decision-making and procedural accuracy are critical.1 Coaching can enhance preparedness and outcomes in these high-pressure, time-sensitive situations.
- Additionally, 9% of physicians see value in coaching for non-procedural skills like diagnostic decision-making and patient communication. Training related to diagnostic accuracy, breaking bad news, patient communication, and teamwork is increasingly sought after and recognized for its impact on patient outcomes and overall care quality. Physicians increasingly recognize the impact of soft skills on outcomes, and coaching may help address blind spots in these areas.
A Sermo member working in Anesthesiology commented: “My hospital isn’t pediatric, but in the emergency room, they can, based on the degree of urgency, admit children. I intubated children when I worked in a hospital where ENT surgery was practiced but in the operating room and not in emergency. I’d like to fill this gap.7”
This highlights how physicians want to close gaps in their own training. Physician coaching offers a safe, supportive framework to self-identify and address these gaps, even when formal training opportunities are limited.
What’s preventing the adoption of pre-procedure physician coaching?
Despite increasingly common examples of its benefits, pre-procedure coaching isn’t yet a widespread practice across healthcare. Available research indicates that pre-procedure physician coaching is uncommon in current medical practice. In a survey of staff obstetricians and gynecologists, only 8% reported having received formal training in coaching techniques. Furthermore, 67% of residents stated that pre-operative goals were “rarely or never” set, and coaching of non-technical and cognitive skills “rarely or never” occurred before procedures.
According to a Sermo poll, the top barrier to JIT being used is a reluctance to change pre-existing workflows, which was cited by 26% of physicians.1 Many healthcare practices have defined routines that, if even slightly changed, can feel disruptive. This highlights that adoption of JIT is as much cultural as logistical, and support to get these programs off the ground requires buy-in from everyone in a care team.
Time pressure is another significant concern. With 24% of physicians citing limited time between procedures as a barrier,1 it’s clear that even short interventions like just-in-time coaching can feel unmanageable in a physician’s busy schedule.
Additionally, coaching programs are not universally available, and access often depends on workplace resources or geographic location. Many physicians lack opportunities for coaching outside of large institutions or urban centers.
There’s also a shortage of trained coaches. One in five physicians said the lack of experienced clinicians to deliver coaching is a limiting factor1.
Cost and skepticism play a role as well. 19% of physicians on Sermo raised concerns about resource allocation and 11% expressed doubt about coaching’s effectiveness.1 Without clear, evidence-based outcomes, decision-makers may struggle to justify investment.
As one Sermo member and physician in Family Medicine put it, “I do feel that coaching could enhance outcomes, but experience leads to having solutions when all hell breaks loose.7” For many, coaching may offer a way to expand that experience safely to support more confident, capable decisions in the moments that matter most.
While demand is present, the infrastructure can be lacking, highlighting the need for more formal coach training or scalable digital alternatives. For coaching to succeed, it must be fast, practical, and easily implemented into existing workflows.
How to implement pre-procedure coaching to be most effective?
When asked what would help make coaching more feasible, physicians on Sermo had clear answers:
- Coach training programs (27%)1: There’s demand for a more formal structure. Senior clinicians need to be equipped not just with technical expertise but with the skills to coach effectively.
- Scheduling flexibility (21%)1: Without dedicated time, coaching remains aspirational. Protected time slots could enable practical adoption without disrupting care delivery.
- Evidence and outcomes data (22%)1: More physicians want to see hard data on cost-effectiveness and patient outcomes. Building this evidence base is key to wider institutional support.
- Technology as a supplement (16%)1: Virtual coaching tools and AI-driven support are welcome but not yet a central solution. They’re viewed as useful add-ons to human-led coaching.
- Organizational policy change (13%)1: Culture and policy must align. Coaching will only thrive when it’s prioritized at the organizational level, not left to individual motivation.
From training coaches and allocating time to demonstrating measurable outcomes and embedding coaching into policy, the path to success lies in treating coaching as a critical component of clinical practice.
To successfully implement just-in-time (JIT) coaching, several structural supports must also be in place.
- Structured, multi-modal curriculum
A pilot study on pediatric subspecialty fellows, using didactics, role-play, and bedside coaching, improved their ability to deliver difficult news, conduct family conferences, and respond to emotions. Both self-efficacy and communication skills increased.
- Deliberate practice and feedback
In the same pediatric subspecialty study, fellows received repeated practice and structured feedback during bedside coaching sessions. Six months post-intervention, improvements in communication skills were sustained, highlighting the value of ongoing feedback and practice.
- Specialty-specific matching
The SCOPE program at four US academic medical centers paired surgical coaches and coachees. Surgeons reported greater satisfaction and higher recommendation rates when their initial sessions were excellent, goals were clearly defined, and specialty alignment was strong, underscoring the importance of relevant matching.
With the right infrastructure in place, coaching can become a scalable, sustainable tool for improving performance, confidence and patient care.
The takeaway
Pre-procedure coaching helps physicians manage daily challenges, such as limited time, managing uncommon procedures, and high-pressure decisions. When implemented effectively, it boosts confidence, reduces errors, integrates smoothly into workflows, and lowers costs.
Despite its benefits, many physicians haven’t adopted coaching due to a lack of institutional support, trained leaders, and dedicated time. Without these structures and more clinical evidence of its value, coaching remains underutilized—not because of resistance, but because it feels impractical.
With proper support, just-in-time coaching can enhance patient care by quietly guiding junior doctors through rare procedures and providing experienced physicians with reassurance during stressful moments. In a field that demands trust and precision, pre-procedure coaching is a practical step toward safer and more confident practice.
As one physician in Family Medicine put it best, pre-procedure coaching “seems like common sense to me.7”
Join the conversation on Sermo
Join 1+ million global physicians on Sermo: a private, verified community where doctors share real-world experiences, debate clinical practices and shape the future of medicine.
Doctors can try it for themselves today and begin to contribute insights via surveys, case studies and discussions on current topics with doctors worldwide.