When Sermo asked physicians if their patients had brought up mouth taping for sleep apnea, more than a quarter (27%) said yes. Another 25% hadn’t seen it directly but had noticed the public discussion, while 46% hadn’t encountered it at all. In other words, this trend isn’t yet a mainstream clinical issue, but it’s breaking into exam rooms fast enough to demand attention.
Mouth taping itself is a simple idea: people place adhesive tape over their lips at night to force nasal breathing. Advocates say it improves sleep, reduces the chance of snoring and can even give cosmetic improvements. As one GP on Sermo explained: “Patients frustrated by sleep issues are trying these viral trends.” So its appeal is obvious, especially for patients desperate for a solution to poor sleep.
That appeal meets the powerful engine of TikTok, where the hashtag #mouthtaping has surpassed 24 million views. Celebrity endorsements, from the likes of Gwyneth Paltrow and broadcaster Julia Bradbury, have further fueled interest. But experts have been quick to raise doubts. While nasal breathing is beneficial, experts caution that forcing it with tape could be dangerous and that current research is limited and inconclusive.
So, do physicians believe mouth taping is worth the hype? This article looks at Sermo poll data and community commentary to find out.
Why are physicians concerned about mouth taping?
The Sermo poll shows just how divided physicians are on mouth taping. Only 8% consider it harmless. A cautious 11% think it might be beneficial if used correctly, but almost four in ten (39%) say it’s potentially dangerous and nearly a quarter (24%) dismiss it outright as pseudoscientific. About one in five (19%) admitted they weren’t familiar enough to judge. On the balance, the overwhelming tone is scepticism, with most physicians focusing on the risks rather than the supposed benefits.
That scepticism is rooted in what taping could conceal. More than 60% of surveyed physicians believe it could delay the diagnosis of a sleep disorder (19% said yes, while 42% possibly). The logic is that mouth breathing at night is often the body’s way of compensating for nasal obstruction or obstructive sleep apnea (OSA). As experts suggest, suppressing that signal with tape doesn’t solve the problem and instead possibly even hides it, increasing the chance that a serious condition will go unnoticed and untreated. Patients with untreated or severe OSA are particularly vulnerable to perioperative respiratory failure and hypoxemia, which requires careful tailored anesthetic and postoperative management, and thus it’s a condition that needs to be diagnosed and treated in an evidence-based manner.
The frustration this creates is plain in the Sermo community’s commentary. “This trend is ridiculous. I can’t believe how much influencers have pushed this trend,” wrote one internist. Others were especially direct about the dangers, with one otolaryngologist stating, “Might as well put a pillow over your face and suffocate yourself.”
And yet, not every physician rules it out completely. One anesthesiologist commented that “mouth taping may be useful in certain situations, but its potential side effects may outweigh the benefits.” This cautious language shows the tension well: physicians generally recognise the health benefits of nasal breathing, but they reject the leap to include it in practice at the moment without further research.
That’s where the debate circles back to the evidence gap. As sleep physiologist Stephanie Romiszewski told The Guardian, there’s “no good evidence yet regarding mouth taping.” The few studies that exist use small sample sizes that give flimsy datasets, hence clinicians are defaulting to the status quo.
The takeaway here is that physicians may not agree on whether mouth taping has any niche potential, but they do agree on the broader point. Until there’s robust evidence and proper evaluation, mouth taping remains, in their eyes, an unsafe shortcut rather than a solution.
Why are people taping their mouths?
When Sermo asked physicians what’s driving the mouth taping trend, the answer was overwhelming: 63% pointed to social media. Platforms like TikTok are driven by emotionally charged content that can often make complex issues overly simplified, so health misinformation often spreads there long before evidence can catch up.
Doctors see the consequences of this every day. As one pathologist put it, “Social media is powerful… people do things without proper research.”
Yet an idea simply going viral doesn’t explain why patients are willing to try mouth taping, something that carries risks. 14% percent of physicians in the poll said the driver was sheer desperation for sleep. For people who are exhausted and searching for relief, even a risky shortcut can feel worth it if the reward could be a good night’s sleep. As one GP put it: “People read on social media of this practice and they believe in it.” In moments of fatigue, many people are drawn in by the promises from influencers, which can sound more convincing than the cautious and nuanced medical advice.
Beyond personal desperation, there are also systemic factors that are influencing the rise of mouth taping. Nine percent of physicians cited mistrust in medicine, while six percent pointed to barriers to care. Some patients feel dismissed or unable to access specialists and so they experiment with DIY methods instead. As one pathologist reflected: “Unless you can analyze research, it’s hard to spot bad advice.”
Taken together, the poll and commentary reveal three layers driving mouth taping: cultural forces that amplify current trends, personal desperation that makes patients more vulnerable and systemic gaps that leave them looking outside traditional medicine for answers. In that sense, mouth taping highlights the widening space between what patients need and what medicine is currently providing.
What do physicians recommend?
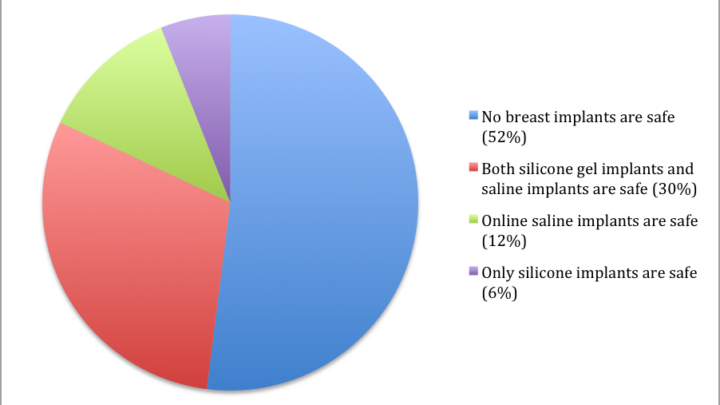
When Sermo asked doctors if they’d recommend mouth taping, nearly half (49%) said never. Another 18% were unsure, while smaller groups allowed for conditional use: 16% under monitoring, 12% with specialist support and just 5% depending on patient history. The numbers show the clear pattern that most physicians aren’t willing to endorse the practice, and those who do so only in tightly controlled circumstances.
Instead, physicians on Sermo stress that patients presenting with mouth breathing or sleep concerns should be evaluated properly. That means ruling out nasal obstruction, allergic rhinitis, or undiagnosed sleep apnea, often through referral to ENT or a formal sleep study. As one ENT put it bluntly: “If you can’t breathe through your nose and then you tape your mouth, now you can’t breathe at all.”
But rejecting the trend is only half the job. Physicians also emphasise the importance of communication, both in the clinic and in the public sphere. In clinics, this means having non-judgmental conversations with patients that lay out the lack of strong evidence and the real dangers, from CO₂ retention to suffocation. As one pediatrician admitted, “I grow weary of debunking social media medical advice,” but the work is essential. Beyond the clinic, many argue for a more active role in public discourse: issuing clear warnings, posting simple explainers online, and partnering with health organisations to reach patients where misinformation spreads.
Crucially, physicians also highlight the need for empathy. As one GP put it, the best way forward is to “respond with curiosity and compassion to keep patient trust while gently confronting harmful behaviors.” Meeting patients halfway, with safer alternatives like allergy treatment or sleep hygiene adjustments, protects both trust and health.
Finally, physicians agree that better evidence is needed. “We need more studies,” said one internist, echoing many. Until then, the advice physicians would tend to give patients is: don’t tape, get evaluated and trust the current medical advice, not TikTok.
Your takeaway
Mouth taping may be popular online, but physicians on Sermo are united in caution.
Most view it as risky, with concerns that it could mask sleep apnea or create new breathing problems. Mouth taping results clinically simply aren’t there, and until robust studies emerge, doctors agree it’s not a safe solution.
What’s driving the trend is less science and more social media, patient desperation and even gaps in trust.
The task for physicians is twofold: evaluate sleep issues properly and meet misinformation head-on with empathy, clarity and evidence patients can trust.
Join the conversation on Sermo
What’s your view on the mouth taping trend? Are patients asking you about it, and how are you responding?
Join the conversation on Sermo now to see how colleagues across specialties are approaching the issue, and add your perspective to the debate.