A staggering 79% of physicians feel moderate to significant emotional distress following a medical error. Our Sermo poll captures the burden of what all physicians face sooner or later: making a mistake. Adverse events affect 1 in 7 patients, with half of all clinicians involved in a serious event at least once. In the U.S, over 300,000 deaths annually are a result of diagnostic errors.
The emotional toll after a medical error, known as second victim syndrome or second victim phenomenon, affects healthcare professionals across all specialties. However, it remains one of the most under-discussed aspects of medical practice. While patients are rightfully considered the primary victims of adverse events, healthcare professionals themselves often become secondary casualties, struggling with guilt, anxiety, and professional self-doubt.
This article reveals experiences from Sermo members across dozens of specialties as they share candid experiences about the aftermath of adverse events, the complex emotions that follow, and the inconsistent support they receive from their institutions.
If you’re seeking perspective, peer connection, and practical coping strategies, continue reading to learn about the steps you can take to go from failure to growth.
Understanding second victim syndrome
Second victim syndrome refers to the emotional impact experienced by healthcare workers involved in medical errors. The second victim phenomenon is not rare; it’s an expected reality in the complex medical system where uncertainty, time pressure, and incomplete information are constant challenges.
Sermo poll insights illustrate the significant impact, as 38% of physicians reported experiencing significant emotional distress after a medical error, while 41% experienced moderate distress. 15% rarely felt distress, and only 4% said they had never experienced emotional distress. As a Sermo member and gynecologist explains, “We carry the burden of our mistakes for years.”
The emotions themselves are layered and often overlapping. 20% reported guilt, another 20% reported anxiety or fear of future errors, 18% cited loss of confidence, 14% felt grief or sadness, 13% reported anger or frustration, 6% experienced depression, and 5% felt professionally isolated. These reactions are common and rarely occur in isolation.
Guilt can deepen anxiety, fear of recurrence can chip away at confidence, and grief can surface months later, triggered by a similar case. Over time, this mix can erode well-being and clinical confidence, especially without structured support.
What physicians feel after an error
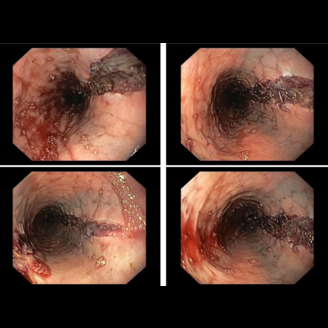
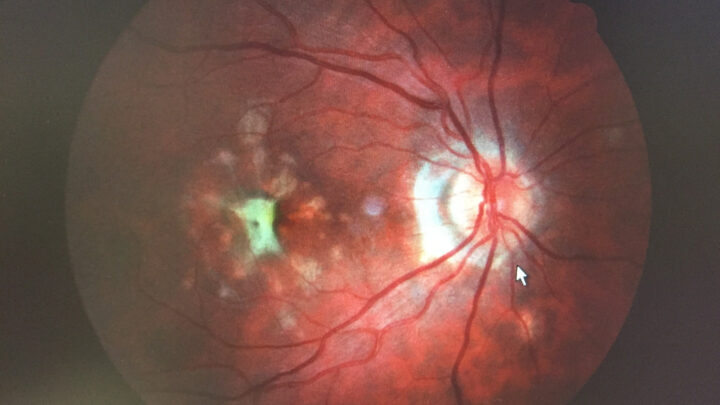
The most common type of medical error is misdiagnosis, which includes failure to diagnose, incorrect diagnosis, or delayed diagnosis. The emotional toll of medical errors aligns closely with the broader stress patterns affecting physicians today. A recent Sermo survey reveals 88% of physicians reporting feeling overworked at least occasionally, and 53% experience this “all the time” or “most of the time.”
On Sermo, physicians describe a spectrum ranging from acceptance to lasting trauma. “We need to forgive ourselves,” shared an internal medicine doctor. A pathologist added, “Errors are inevitable in the course of human events.”
Others frame mistakes as growth, as one radiation oncologist said, “Mistakes are a form of growth.” Yet the lingering impact is also clear, with a reproductive endocrinologist reflecting, “The impact stuck with me for a long time.”
These voices reveal a paradox. Many clinicians intellectually accept that errors occur, yet emotionally struggle to reconcile their professional identity with the outcome. That friction can fuel rumination, sleep disturbance, and hypervigilance, which in turn affects team dynamics and patient interactions. To exacerbate the situation, the National Academy of Medicine details how healthcare blame culture, fear of litigation, and stigma can compound distress, delaying recovery and discouraging open learning.
Where support fails and what’s needed
“There is no support. Just lawsuits,” highlights an internal medicine doctor. Sermo community insights also indicate that formal support is lacking, as only 15% of physicians reported being fully supported by their institution. In comparison, 28% didn’t receive any support whatsoever.
Broader systemic issues in healthcare funding compound the challenge of inadequate institutional support. Recent federal mental health funding cuts have left 72% of physicians anticipating significant negative impacts on patient care, particularly affecting vulnerable populations who rely on these services. This reduction in mental health resources creates additional strain on physicians who are already struggling with second victim syndrome, as they may have fewer avenues for professional counseling and support services.
When asked what kind of support physicians wanted, they identified institutional acknowledgement (23%), structured reflection (18%), and peer forums (15%) as the most requested forms of assistance. This study demonstrates how perceived institutional support for second victims can lower emotional exhaustion in physicians and create a better culture of safety.
An orthopedic surgeon and Sermo member explained, “The hospital did not support me, but rather blamed me.” A family medicine physician added, “Assistance in this regard is likely under-resourced.” while an emergency medicine physician concluded, “The most important resource is teamwork.”
The data shows a gap: many clinicians experience emotional fallout after medical errors, but responses from institutions are often limited or inconsistent, negatively affecting both physicians and the patients they treat.
From guilt to growth: how physicians recover
As a Sermo member and dermatologist puts it, “If you don’t make mistakes, you’re not human.” But how are physicians supposed to pick up the pieces and grow from mistakes?
Recovery is not linear. On Sermo, many physicians describe a sequence: shock, self-questioning, finding meaning, and, eventually, integration into practice.
52% of surveyed physicians said their experience initially caused distress but eventually led to professional growth. 24% said it positively changed their practice. 10% reported long-lasting emotional and professional setbacks, while 11% said it had no long-term impact.
Support processes, such as peer teams, quick debriefs, open case reviews, and confidential counseling, can help ease distress and enhance learning. When leaders recognize the human impact and encourage seeking help, clinicians recover faster and feel safer at work.
Physicians can recover and grow from medical errors and adverse events in healthcare through implementing a standard procedure:
Step 1: Care for the patient and family
When medical errors occur, physicians should explicitly state that an error happened, explain its details and impact on the patient’s prognosis, discuss why it occurred, outline steps to prevent recurrence, and offer an apology.
Step 2: Report to appropriate sources
Practitioners must ethically inform patients and the care team about significant clinical oversights. This critical communication handles immediate negative patient outcomes and prevents further mismanagement. Documenting and reporting errors are essential for patient safety, aiding other providers, and improving hospital-wide measures.
Step 3: Review the incident
Post-event debriefing, whether immediate or delayed, facilitates future learning in a non-punitive environment. While beneficial for improving medical practice with peer input, it differs from a root cause analysis, which a risk management team conducts. Both identify event-related challenges for further discussion.
Step 4: Manage legal issues
Over 60% of U.S. physicians face lawsuits, a demanding and confidence-eroding process. Seek legal advice from employer/insurer-identified attorneys, and for emotional support, consider professional counseling to manage this stressful experience.
Step 5: Engage in self-care and stress management
Doctors affected by patient errors or deaths, especially sudden ones, should seek grief support. Though accustomed to adverse events, physicians must balance compassion with emotional distance. The medical culture of emotional suppression needs to change, as deep impact from patient trauma or death can occur at any career stage. Learning how to forgive and reframing can help to unpack adverse events mentally.
Physician peer reflections further illustrate this arc. “You reflect on the mistake each time you perform the procedure,” noted a dermatologist on Sermo. A general practice physician described medical errors as “a way of learning more things.” “We grow when we learn from mistakes,” said an anaesthesiologist, while an orthopedic surgeon added, “Wisdom is often a product of prior failures.”
Overall, these approaches emphasize emotional healing, ethical transparency, continuous learning, peer support, and professional growth to enable physicians to recover from medical errors and ultimately improve patient safety and care quality.
Even small but consistent support processes, like a direct note from leadership acknowledging the event and offering resources, can change the trajectory for a clinician who might otherwise retreat into isolation. When physicians have time and support for reflection, they’re better equipped to process adverse events constructively rather than getting trapped in cycles of self-blame.
Breaking the silence
Breaking the silence around medical errors requires shifting from individual blame to collaborative learning models that have proven effective in other areas of healthcare. Collaborative care approaches, which emphasize interdisciplinary teamwork, shared responsibility, and open communication, offer a framework for addressing second victim syndrome systemically.
To prevent the second victim phenomenon from becoming a career-defining burden, physicians on Sermo repeatedly call for transparency, humanity, and cultural change. A pediatrician shares on Sermo, “The expectation is perfection, which is doomed.” A general surgeon added, “We all have different levels of emotional resistance; we need to support each other.” An infectious diseases physician and Sermo member urged, “Let’s change this toxic culture.”
Silence perpetuates the second victim syndrome cycle. Open discussion reframes errors as system signals rather than individual failings.
Key takeaways
Most physicians will experience emotional fallout from a medical error at some point in their career. The insights and shared experiences from Sermo members make the pattern clear: guilt, anxiety, grief, and loss of confidence are common, but institutional support is inconsistent.
Still, growth is possible and likely when clinicians have space to reflect and communities that respond with empathy and action.
Clinicians can start by acknowledging the emotional impact of adverse outcomes, both their own and their colleagues’. Normalizing peer reflection and learning from mistakes reduces isolation. Institutions should be encouraged to develop or adopt structured, non-punitive support pathways. Sharing coping strategies, stories, and systems that helped recovery can help others do the same. Communities like Sermo offer a secure space for reflection and healing.
People all make mistakes. The danger is not in the error, but in silence, shame, and isolation. Talk about it with physician peers who get it.
Join the discussion on Sermo
How do you cope with the emotional fallout of medical errors?
What support would you offer a peer experiencing guilt or grief?
What systems have helped, or failed, you in the past?
Share your story, read about others, and join a community committed to honest and compassionate conversations about the realities of modern practice.