Collaborative care models: what are they, their benefits & examples
Physicians today face growing challenges—fragmented care, increasing burnout, and time constraints. Collaborative care models streamline workflows, enhance patient outcomes, and foster interdisciplinary teamwork, leading to improved efficiency and job satisfaction.
What is collaborative care in healthcare?
Collaborative care models in healthcare are structured systems that integrate the care provided by healthcare professionals with various roles and disciplines to provide patient-centered care, leading to better efficiency, improved outcomes, and increased patient satisfaction. Every physician has faced a challenging case where collaboration made all the difference. From chronic pain management to complex comorbidities, interdisciplinary teamwork isn’t just helpful—it’s essential.
This guide explores how collaborative care models are reshaping healthcare, providing real-world physician insights and actionable strategies to implement them in your practice. A doctor from the Sermo community says “I want to share a case that highlights the importance of collaborative care in managing chronic pain. Mr. Smith, a 45-year-old patient, has been dealing with persistent lower back pain for several months… Collaborating with specialists such as a physical therapist and pain management expert, we developed a multimodal treatment plan tailored to Mr. Smith’s needs.”
For many patients, traditional healthcare often falls short. Fortunately, collaborative care offers a fresh start, a patient-centered, team-based approach designed to fix common gaps. This unique and effective approach puts the patient at the center, supported by a team of professionals working together toward one common goal – your overall health and well-being. Collaborative Care Models are highly effective for managing complex conditions by integrating primary care providers, specialists, and care management to address the needs of each patient.
Another doctor on Sermo noted the following: “Numerous case studies and expert opinions underscore the significant benefits of collaborative care models in managing FCS. For instance, a detailed case study involving a multidisciplinary team demonstrated marked improvements in patient outcomes, including dramatically reduced triglyceride levels and a notable decrease in the frequency of pancreatitis episodes. This comprehensive care approach not only enhanced patient well-being but also provided a framework for integrating various treatment modalities effectively.”
Several key principles make collaborative care successful.
Patient-centeredness
Patient-centeredness is about putting patients first by tailoring healthcare to their individual needs. Physicians need to focus on what matters most to the patient, remembering that each person is more than just a diagnosis. This approach allows a team of professionals, along with the patient and their family, to collaborate to prioritize the individual needs and preferences of the patient to provide the most comprehensive care.
Interdisciplinary collaboration
A team of health professionals from various backgrounds works together to provide care. This approach improves patient outcomes, reduces medical errors, and lowers healthcare costs. As health professionals bring their unique expertise and perspectives, they can create personalized care plans that treat the whole patient through the sharing of information, coordinating care plans, and tracking of progress. With effective communication, clear protocols and workflows are developed.
Data-driven decision-making
Data helps track patient progress, identifies trends, and improves treatment effectiveness to help guide the team toward better outcomes. By relying on facts and insights, a team can work together to make better diagnoses and prescribe effective treatments. This helps personalize the treatment plan, allowing for adjustments. If a treatment isn’t working, the data will show it. The team is then guided toward making sure the patient is on the best path.
Measurement-based treatment
With measurement-based treatment, a team can effectively track progress by using standardized, valid, and repeated measurements to see how a patient is doing. Standardized measures help to track progress and allow for the evaluation of treatment. It leads to better treatment outcomes by ensuring that interventions are effective and responsive and promotes precise communication between patients and physicians. Patient-reported outcome measures are questionnaires or other tools that clients complete to report their symptoms and experiences, while clinician-reported outcome measures are used to assess patient progress.
Evidence-based care
Evidence-based care relies heavily on research. By using the best research evidence combined with the expertise of the medical professionals and the patient’s needs, beliefs, and goals, evidence-based care can lead to better health results, reduced complications, and increased patient satisfaction. It also allows providers to deliver more effective care and encourages everyone to make informed decisions based on scientific evidence rather than tradition or personal opinion. Significant research spanning three decades has identified the Collaborative Care Model as the most effective and efficient in delivering integrated care.
Accountable care
The goal of accountable care is to improve the quality of care and improve patient outcomes by focusing on prevention, wellness, and efficient care delivery. It is measured by patient satisfaction and cost of care – key metrics that help determine the effectiveness of the care provided. Accountable care improves patient outcomes and reduces costs through shared savings programs, where providers are accountable and reimbursed for quality and not just the volume of the care provided.
Why collaborative care models matter
Collaborative care models bring a patient-centered approach by integrating various healthcare providers to promote communication, share decision-making, and coordinate interventions to improve the quality of care and optimize patient outcomes. There are several benefits.
Improved mental health amongst healthcare professionals
By integrating mental health services into primary care and emphasizing teamwork, the mental health and well-being of healthcare professionals are greatly improved. Stress and burnout are reduced by helping to divide the workload among various team members and easing the burden on individual providers.
Options for more holistic and innovative treatments
With traditional healing practices finding their way into contemporary medicine, it allows for more innovative treatment plans. In the past, pain medications were widely prescribed to manage chronic pain. These habit-forming prescription painkillers have led to a major crisis, with millions of Americans becoming addicted to opioids. Whole-person approaches to health utilize alternative practices such as acupuncture and chiropractic care to reduce pain without relying on prescription medications. Patients are taught self-soothing techniques for pain management to avoid the risk of addiction.
Lowered health care costs
Millions of people in the United States are struggling to afford quality healthcare, causing them to delay or even avoid medical treatments, prescriptions, and preventative care. Collaborative care models work to make care more affordable by cutting down on overhead costs. Preventative, whole-person healthcare lowers the cost of healthcare by reducing the need for more costly future treatments.
Better outcomes for a diverse patient population
When mental health care is reduced, it goes a long way in helping low-income patients who would otherwise struggle to afford the treatment they need. Collaborative care models are cost-effective and may be covered by Medicaid or Medicare.
Higher quality care
With collaborative care models, patients have reported a higher satisfaction rate. Mental and physical health are closely related, making it crucial for a healthcare system to address both and allow patients to actively participate in their treatment plan. The workload is better distributed among a care team, and providers are more able to provide individualized attention, leading to better patient outcomes.
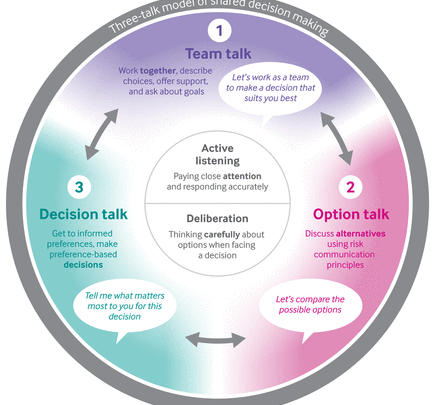
Better communication between specialties
Collaborative care models allow for better, more streamlined communication among patients and providers. When a patient sees different doctors, communication becomes difficult; however, when a care team works together and has regular interaction, it leads to better communication and care management. In addition, patients have a higher level of input when it comes to their treatment plans and medical decisions.
Key components to build a collaborative care model
Interdisciplinary teams
Comprehensive care requires a team of professionals from various disciplines, including physicians, nurses, allied health professionals, social workers, and therapists. This allows for open communication and collaboration to make informed decisions.
Technology integration
A collaborative care model is enhanced through technology by leveraging digital tools to help facilitate communication, data sharing, and remote support to ultimately improve the outcome for patients. Using electronic health records, telecommunication technologies, and clinical decision-support tools can help reduce errors and promote adherence to evidence-based guidelines.
Shared responsibility
Clearly defined roles and shared goals are vital. Professionals leverage their expertise to provide comprehensive care, ensuring efficient and effective care delivery.
Patient engagement
Patients are actively involved in the decision-making process, and their preferences and values are considered alongside clinical recommendations.
How to implement collaborative care models in your practice
Collaborative care models can be implemented into medical practice by taking the necessary steps.
Establish regular case meetings
Interprofessional communication in healthcare is growing increasingly complex, and according to a survey conducted by Sermo, over 31% of providers feel ill-equipped to train staff in emerging technologies. Regular case meetings help to foster communication and ensure that everyone is on the same page. It is important to review patient progress and adjust treatment plans as needed.
Clearly define team roles
Identify core team members and outline all responsibilities. Be sure to create effective communication protocols by using secure messaging for quick updates. Always keep shared documents organized to prevent miscommunication and make things efficient. Every member of the team brings unique skills, so the team should include a primary care physician, a care manager, and consulting specialists.
Encourage cross-specialty collaboration
Always build trust by encouraging open communication, valuing the input of each member, and creating a culture of respect. It is important to establish a shared purpose by ensuring all team members understand the goals and objectives of the model, aligning their efforts towards a common vision.
Collaborative care vs integrated care
Collaborative care and integrated care both focus on teamwork and improved patient outcomes, however, integrated care is a much broader concept that encompasses the integration of various healthcare services. Collaborative care is a specific model within integrated care that puts the focus on a team-based approach to mental health care in primary care settings.
The bottom line of collaborative care models
Collaborative care models go a long way in improving patient outcomes. The model emphasizes open communication among healthcare providers and caters to the individual needs of each patient. Collaborative care models improve patient outcomes through effective communication and shared decision-making, minimizing the risk of errors and improving patient safety. It allows patients to feel more empowered by being actively involved in their treatment plan and also prevents hospital readmissions, minimizes unnecessary tests and procedures, and improves patient compliance, reducing costs as a result.
Sermo’s physician-only community provides a dedicated space for doctors to exchange insights and shape the future of collaborative medicine – with more than 50,000 patient cases solved last year alone. When an interdisciplinary team works together, it allows for stronger relationships and improved outcomes for everyone. And, Sermo is completely free. Create an account today.