Virtual reality (VR) is no longer limited to entertainment or gaming. Over the years, it has revolutionized multiple industries, and one of the most exciting frontiers ripe for transformation is medicine.
Healthcare professionals are perpetually seeking ways to enhance patient care, maintain their education (CMEs), and stay up to date. VR is stepping in to bridge the gap between education, access, and real-world skill-building. We polled our Sermo members to get relevant insights on the matter, and a resounding 69% of physicians agreed that VR offers immersive simulations that are better for learning than traditional methods alone.
But how exactly does VR impact medical training, and what does this mean for new and veteran physicians? Let’s explore the growing role of VR in medicine, including its current applications, widespread benefits, and upcoming challenges.
The role of VR in medical training
Virtual reality has become a game-changer for training medical professionals, especially as patient treatments continue to grow in complexity. An overwhelming 68% of surveyed physicians agree VR should be an integral part of medical education. Unlike traditional learning with textbooks or cadavers, VR is a technology that creates immersive, 3D interactive environments for real-time problem-solving.
As a General Practitioner on Sermo discussed “Virtual reality has the potential to revolutionize medical education by offering a dynamic, immersive and hands-on approach to learning, this technology provides unprecedented opportunities for hands-on training and skill development in the healthcare field, which can have a significant impact on the training of highly trained and competent health professionals. Limitations: Equipment and techniques.”
Here’s how VR is reshaping medical education for today’s practitioners:
1. Hands-on learning without risks
VR offers an effective hands-on training solution without requiring direct interaction with patients. Virtual environments simulate risky real-world medical scenarios, allowing physicians to practice new techniques, test their knowledge, and safely learn from mistakes.
Consider VR tools for delicate surgeries, where learners can manage complex cases step-by-step, error-free.
2. Reducing patient risks through simulations
Medical errors are a significant public health issue, according to the CDC, in the US and in many countries globally and inadequate training can play a role. With VR, physicians can fine-tune skills or rehearse rare, high-stakes procedures before encountering them in real life. By the time they’re face-to-face with a patient, they’re confident and prepared.
3. Bridging the gap between theory and practice
While theoretical knowledge is critical, it’s practical application that truly builds expertise. VR bridges that knowledge gap. For instance, physicians could diagnose rare or unusual symptoms in virtual patients or receive immediate, detailed feedback on how well they followed leading protocol standards.
Key applications of VR in medical training
The early twenty-first century, referred to as the “VR Winter,” saw limited public interest and ongoing research primarily in corporate, academic, and military settings, hindered by high costs and fragile infrastructure. However, around 2011, renewed consumer interest in VR for entertainment emerged, driven by key technological advancements from companies like Valve, NVIDIA, and Oculus, making HMD-based VR accessible to a broader audience.
The Covid pandemic highlighted the growing importance of telehealth and emphasized the necessity for remote learning in medicine. The potential of VR in healthcare is extensive. A third of surveyed doctors on Sermo reported that anatomy and physiology education could benefit the most from VR training. Surgical procedures training was the top pick, perfect for VR skill-building, and earning 42% of the vote. From clinical skills to cognitive decision-making, here are some standout applications of VR tools in advancing medical training:
Surgical training
Surgery is an intense discipline where precision and practice go hand in hand. At Mass General, Orthopedic students are already practicing VR surgeries. According to Dr. Augustus D. Mazzocca, chief of sports medicine at Massachusetts General Hospital and faculty member at Harvard Medical School, the hospital uses a system called PrecisionOS to augment orthopedics and train medical students and residents in the motor skills required for surgery.
VR equips surgeons with simulations to refine procedural accuracy using haptic feedback tools mimicking real tissue. This allows practicing surgeons to get practice in on bypasses or transplants with zero patient risk.
Patient diagnosis and treatment
With tools like 3D anatomical visualizations, doctors can better understand a patient’s condition. Additionally, VR supports enhanced, collaborative treatment planning by simulating various outcomes based on diagnostic data across geographical boundaries.
Emergency response training
Time-critical scenarios like cardiac arrest are ideal for VR training modules. Emergency responders can practice maintaining composure while implementing life-saving measures in seconds. It’s also a great way for healthcare professionals looking to get certified to get extra practice in before going live.
Anatomy education
Immersive VR provides detailed 3D anatomy visualizations, effectively aiding students and physicians in learning and specializing in surgical approaches.
As a GP on Sermo commented: “I consider VR to be a great tool for medical study, especially in the branch of anatomy and surgery, since it allows for a broader, more realistic and interactive study.”
Mental health training
Virtual Reality is an emerging tool in the mental health field, particularly notable for its application in teaching students and staff exposure therapy and social skills training. These controlled environments assist in treating conditions like PTSD, anxiety, and phobias.
Pediatric and neonatal simulations
Training physicians in pediatric or neonatal care becomes more intuitive with VR. Handling fragile infants or understanding how to identify and treat rare congenital diseases is thoroughly covered through simulations that mimic real-world medical complexities.
Telemedicine integration
Telemedicine combined with VR-based training allows rural physicians to upskill remotely. Collaborative surgeries or discussions transcending geographical barriers make such technologies invaluable, especially as medical staffing shortages continue to rise.
Endoscopy and minimally invasive procedures
The low-risk practice of endoscopic procedures benefits greatly from VR simulations that mimic extreme precision and accuracy. These tools are particularly helpful in mastering minimally invasive surgery techniques and life-or-death scenarios.
Benefits of VR in medical training for physicians
Can VR training replace tried and true methods? A Pediatrician discussed on Sermo, “VR is helpful for kinaesthetic learning, though will probably complement traditional methods — there is no substitute for hitting the books!” 68% of U.S. medical schools have adopted VR or AR (Augmented Reality), at least in some regard, into their curriculum as of 2024 according to the Association of American Medical Colleges.
Why are so many healthcare organizations and universities betting heavily on VR? The answer lies in its outcomes. Here are some notable benefits driving adoption:
A safe environment for trial and error
Mistakes in VR training are learning opportunities, devoid of life-and-death stakes. Physicians develop competencies faster without fearing repercussions.
The University of Northampton and the University of Oxford already use VR learning platforms to train nurses, medical students, and doctors, with overwhelmingly positive feedback. According to the faculty, “VR simulation allows learners to practice scenarios repeatedly in a safe environment, improving skills and transferring knowledge to practice more effectively.”
Standardized training
One VR scenario delivers consistent protocols and practices to every user, ensuring equality in skill acquisition across medical teams.
Reduced dependency on cadavers
Rather than searching for diminishing cadaver resources, VR offers anatomically accurate simulations, serving as an ethical and reusable alternative.
Scalable, flexible learning
Hospitals can train hundreds of physicians simultaneously via VR compared to limitations posed by equipment or physical trainers.
Enhanced collaboration through multiplayer simulations
Teams from across locations can connect for collaborative surgeries or decision-making exercises, encouraging teamwork between healthcare providers.
Repetition to master rare cases
Training through VR allows doctors to repeat unique or rare procedures, honing their skills until performing with precision becomes second nature.
Customizable learning experiences
Tailor-made VR training modules meet physicians at their learning level, allowing them to upskill without frustration.
Muscle memory development
Repeating VR-based procedural exercises ingrains them into muscle memory, critical for high-stakes surgeries requiring precision.
Time efficiency
A growing number of studies indicate VR training requires significantly less time than older methods, meaning physicians get training results faster.
Boosted confidence
Doctors emerge from their VR training with a heightened sense of preparedness and confidence, essential to executing under pressure.
Challenges in implementing VR in healthcare
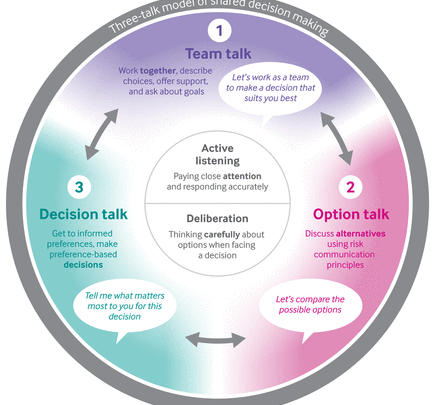
While the promise of VR training is exhilarating, the process isn’t without hurdles. Researchers suggest that successful adoption can be enhanced by using multiplayer scenarios, where teams of nurses and physicians train together rather than working in isolation. This collaborative approach allows learners to practice repeatedly in AR and VR, enabling them to manage stressful situations more effectively by gaining familiarity and confidence through real-time decision-making.
Here are some roadblocks medical organizations must address when incorporating this futuristic tool:
High implementation costs
Sermo’s survey revealed 59% of physicians believe high costs are a limitation for widespread adoption of VR. Prices have dropped significantly from over $35,000 in the early 2000s to under $1,000 in 2025. That said, purchasing VR equipment, subscriptions, or creating custom training modules may be prohibitively expensive for hospitals or education facilities to implement at scale.
Learning curve for new technologies
Resistance to change is common, particularly among staff who are less familiar or uncomfortable with digital tools. Also, older healthcare professionals may struggle adapting to VR systems, requiring added support and introductory training programs. 18% of doctors on Sermo voted technical difficulties as a leading limitation of VR adoption. This includes not only operating the hardware (headsets, controllers) but also understanding the software interfaces and integrating VR into clinical workflows.
Ethical boundaries
A number of ethical dilemmas arise with simulated experiences, especially concerning procedures like euthanasia or abortion. AR/VR in medical training raises ethical concerns regarding patient data privacy, legal implications, user training, and informed consent.
Researchers must adequately train users on virtual assessment procedures and ensure patients understand and agree to how VR is used in treatment protocols. Additionally, patients have varying tech skills, leading to the potential for disparities in healthcare access using VR. Numerous researchers emphasize the importance of ongoing research and monitoring of the ethical implications of virtual reality in healthcare.
Virtual reality could be a healthcare revolution
VR’s transformational impact on medical training is undeniable. Simulation-based learning prepares physicians like never before, bridging knowledge gaps while increasing safety, confidence, and expertise. The feedback from the global medical community has been overwhelmingly positive.
Physicians on Sermo, a thriving network of 1.5 million healthcare professionals, are discussing VR’s potential to enhance learning outcomes while complementing traditional training.
Are you curious how VR and related medical advances are leveling up healthcare professionals worldwide?
People also ask:
VR in medicine enables immersive simulations for surgical training, patient diagnosis, emergency response practice, anatomy education, mental health treatment, and telemedicine integration.
In medicine, Virtual Reality (VR) is a transformative technology using immersive, interactive 3D environments for education, training, research, and therapy. This technology allows learners to engage with realistic simulations, practice procedures risk-free, and experience diverse clinical scenarios, enhancing skill acquisition and patient care.
Virtual Reality (VR) offers a transformative and hands-on approach to education, augmenting traditional methods with immersive and interactive learning. VR enables tangible engagement with complex concepts, promoting deeper understanding and practical application without physical or safety limitations, especially valuable for psychomotor skills and hazardous scenarios. Implementing VR in education promises time and cost savings through repeatable, customizable simulations that reduce instructor time and expensive equipment.
Doctors use VR for surgical training to refine skills without patient risk, practice diagnoses and treatments, enhance emergency response preparedness, mental health training, and anatomy education.