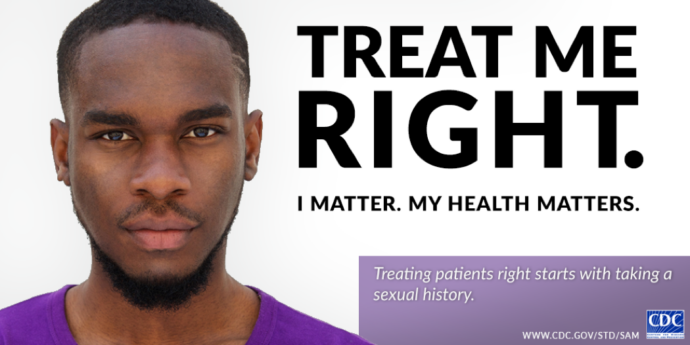
April is STD Awareness Month. Over the month, the CDC has been presenting a series of posts around this year’s theme – Treat Me Right – which focuses on the important relationship between healthcare providers and patients. You’ll hear it here first on Sermo! Last week, Dr. Gail Bolan, director of CDC’s Division of STD Prevention, discussed the importance of a strong patient-provider relationship and highlighted some resources you can find on the STD Awareness Month website. Today, in her second installment of this series, Dr. Bolan talks about the importance of taking a sexual history and gives tips on how to start the conversation.
Let’s talk about sex. And let’s face it, talking about sex can be awkward even for those of us who are immersed in sexual health work on a daily basis. But what we know is that many patients want to discuss their sexual health with you, and most want you to bring it up. We also know that taking a sexual history is essential to providing quality health care. By having these conversations, we help to normalize and destigmatize discussions around sex.
Why should you take a sexual history?
Taking a sexual history allows you to:
• Have a more complete picture of your patient’s health
• Identify those patients who are at risk for STD/HIV
• Identify the appropriate anatomical sites for STD testing
• Provide an opportunity for risk reduction counseling
We have tools to help you
The Provider’s guide from the National Coalition of Sexual Health is a fantastic resource that was recently released. It was created to help health care providers like you better incorporate sexual health discussions and recommended preventive sexual health services into both adult and adolescent patient visits.
The guide:
• Offers tips for having a productive sexual health conversation
• Highlights the essential sexual health questions you should ask of both adults and adolescents
• Provides questions you can ask your adolescent patients that address puberty, sex, and gender identity and sexual orientation
• Includes tables of recommended (and not recommended) preventative sexual health services
Tips to help you talk about sexual health with your patients
• Ensure confidentiality, especially among your adolescent and young adult patients.
We hear time and time again that one of the top reasons that youth don’t seek out STD care is out of fear that their parents will find out.
• Assess your own assumptions, feelings, and reactions.
Many patients worry that their health care provider will judge them, treat them poorly or make them feel unwelcome if they reveal their sexual identity or sexual behavior.
• Ask about sexual health prior to the visit.
One way to discreetly introduce the topic of sexual health is by incorporating it into your patient questionnaires.
• Help normalize your sexual health questions and STD/HIV testing recommendations.
Let your patients know that you ask these questions and offer these services “to all my patients, as sexual health is a normal part of a person’s overall health and well-being.”
• Use inclusive language.
Heterosexual orientation or gender of a patient’s partners should never be assumed. Use gender-neutral terms such as “partner”. Ask your patients what pronoun they prefer.
Sermo wants to know: Do you have a method for breaking the ice when it comes to discussing patients’ sexual health or history? Login or join Sermo to participate in this conversation!