59% of patients associate a physician’s bedside manner to the quality of care received from a health care facility, according to a physician survey1. These patients also revealed the importance of compassion, comfort, and patience in their interactions with their doctors. This is particularly important in cancer care because patients react differently to a cancer diagnosis.
Apart from professional competence, certain strategies and skills are necessary to help oncologists provide positive patient experiences. Your ability to connect with your patients can create a positive patient relationship that support better health outcomes. Likewise, demonstrating a positive attitude and communicating professionally typically help patients handle sad news. Here are seven specific bedside manner practices to show your patients how much you care.

1. Embrace collaborative communication
Collaborative communication is a two-way approach to communication that facilitates shared decision-making. Instead of providing information from a standardized cancer treatment protocol, the oncologist strives to provide essential details and seeks feedback from the patient. Also, the oncologist discusses the diagnosis and therapeutic options, keeping the following in mind:
- Level of risk acceptance
- Patient’s needs and expectations
- Outcome preferences
- Associated costs
This approach allows patients’ active participation in their management process. Medical professionals who practice good bedside manner positively impact future patient interactions and the overall patient relationship. Understanding how the patient feels maximizes treatment adherence, which supports better health outcomes.
2. Anticipate and manage emotions
43% of oncologists revealed that fear is the major emotion most patients express during cancer care, according to a 2022 Sermo study2.
Your ability to anticipate a patient’s emotional response before discussing details of a cancer diagnosis typically helps you to manage their feelings. Some patients may express fear, anxiety, or feel depressed after you break the news. However, your communication style and choice of words may influence a patient’s psychological state and patient’s stress level.
A hospital study3on the psychological state of patients who received a cancer diagnosis expressed varying degrees of anxiety and depression. The following factors were associated with lower levels of patient anxiety:
- Preparing the patient for a possible cancer diagnosis.
- Having the family member and friends wanted by the patient present to hear the diagnosis.
- Providing the patient with details of the diagnosis as desired.
- Providing written and clear information specific to the patient’s condition.
- Answering the patient’s questions the same day with easy to understand treatment guidelines based on your medical background and medical knowledge.
- Discussing the patient’s feelings and being reassuring with active listening skills.
Also, patients had lower levels of depression when the oncologists discussed:
- The severity of the medical condition
- Treatment options and recommended treatment plan
- Involv the patient in the treatment decisions
- Clearly explain the medical education the doctor has and how the medical schools and training will help ensure the best possible patient outcome.
Keep in mind, both the information and how you present it may influence your patient’s emotional state.

3. Actively communicate
Effective doctor-patient interaction goes beyond words. Besides demonstrating knowledge in your specialty, cancer patients generally feel better when you are empathetic and listen to them.
Use your voice tone and body language to show compassion and how you genuinely care about the patient. Good bedside manners include mirroring the patient’s body language and showing the patient they have your full attention. Listen attentively to not only the words but also the emotions behind the words spoken. Ask open-ended questions to enable the patients to discuss how they feel, build patient trust and reassure them.
One clinical study4 on intensive care patients revealed that five days of touch reduced emotional stress indicators. A study5 on the importance of touch in clinical consultations revealed that a doctor’s touch on the back of most patients comforted them. Hence, you can show how much you care and comfort your patients with a gentle touch on the back.
Communicating with a calming tone and non-defensive body language also supports a positive patient experience. Doctors should strive to speak professionally and share your medical knowledge, but do not be afraid to show your human side to build patient trust. An important aspect for physicians to remember is to maintain control of the conversation but employ active listening to help alleviate patient concerns and improve their outlook on medicine.
4. Manage patient’s beliefs
Socio-cultural factors influence an individual’s belief system about health care. Some patients may have fear or negative beliefs and perceptions about the medical field that may affect their decision to receive and complete treatment.
An essential part of good bedside manners for doctors is to identify any perceived beliefs your patient has. Then, create opportunities for them to ask questions you can address with research and medical knowledge. Being open to patient interview questions avoids mistakes when the physician assumes desired goals and for them to improve patient adherence to therapeutic plans. Also, explain in detail the treatment options and the benefits as well as the drawbacks.
Aim to understand what and how the patient thinks about the condition and treatment options. Also, seek feedback and tell the patient to briefly summarize what you have told them to assure they understand the condition and are aware of treatment options.

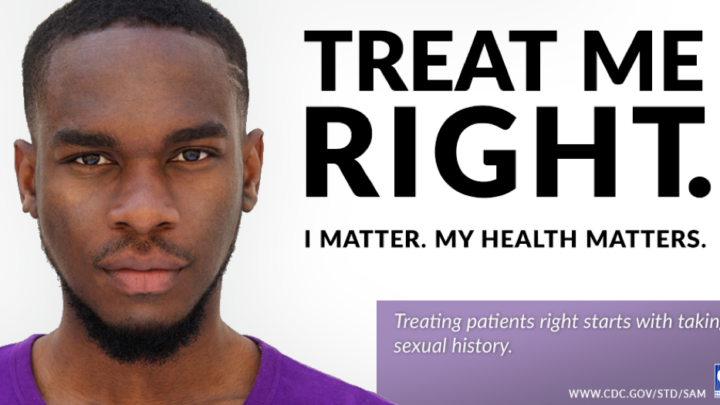
5. Be respectful
Irrespective of your best efforts, you may encounter patients who hold divergent views and disregard your expert recommendations. Also, a patient or their family members may disrespect you even when you have given your best.
Healthcare professionals should aim to stay calm, understand patients’ feelings, and respectfully address the underlying problem. It may take practice but treat each patient and family member interaction as an opportunity to develop good bedside manner.
6. Stay focused
Face-to-face interaction is key to a meaningful interaction and good bedside manner with your patient. Patients feel understood when you focus your attention on them. Make eye contact regularly during your conversations and avoid distractions from technological devices, including medical ones.
Patients seek care and advice from physicians for a variety of issues. Eliminating distraction while in the room, help you to deliver the best possible health results.

7. Create time to check on patients
The average oncologist spends hours consulting in the clinic and may find it difficult to follow up with patients regularly. To help with this, make sure your patients are aware of the next appointment time and when they can expect to hear from you again.
To help optimize your time for checking on your patients, create a system or process that is easily repeatable. For instance, prepare and send a scheduled automated follow-up email for each patient a few days after consultation or use a personal assistant to follow up with your patients.
Barriers to a good bedside manner
Your communication skills play a crucial role in developing a good bedside manner. Here are common communication errors6 that may affect your bedside manners:
- Paucity of information: Instead, provide clear and profound information about the disease, treatment plan, prognosis, purpose of care, expectations, the patient’s involvement in the treatment process, and other relevant details.
- Unaddressed emotions: To resolve this, listen actively to the feelings behind your patient’s words and encourage them to discuss how they feel. Patient’s body language and tone of voice can tell you as much as their words and part of a good bedside manner.
- Monologue type of conversation: To avoid monologue conversations, use dialogues to ask questions and get feedback to keep your patients active in a discussion. A 2022 Sermo physician survey revealed that 77% of doctors prefer a dialogue style of communication.

A good bedside manner differentiates oncologists and medical professionals
A good bedside manner builds patients’ trust in you and optimizes your cancer patient care. Patients express different emotions, and if addressed, this could enhance their health outcome and treatment adherence.
Physicians and any healthcare professional seeking a rewarding career should first seek to understand and reaffirm the human nature in all of us, which is done through providing the best bedside manner possible. When you develop patient relationships, it also makes you feel better as a health care provider.
In addition to your specialized knowledge, showing empathy and compassion through how you communicate with your patients sets you apart from your peers.
To learn more about developing bedside manners, you can learn from other oncologists’ conversations in the Sermo community or participate in virtual tumor boards. Join Sermo for free today to gain access to an online community of experienced physicians.
Footnotes
- Patient Sentiment Report 2022
- 2022 Sermo study
- ScienceDirect
- ScienceDirect
- National Library of Medicine
- National Library of Medicine