Thanks to new technology and the broader industry shift toward value-based care, patient experience models are fast-evolving. Telehealth, interdisciplinary care and improved education all contribute to improving patient outcomes. For example, according to a Sermo poll, nearly 50% of surveyed physicians offer telehealth as part of their practice, and that number is likely to grow in the coming years.
Another Sermo survey revealed that 85% of physicians reflect on the quality of their care frequently or constantly—but only 51% said they were very satisfied with that quality.
Improved patient outcomes have huge impacts on care. Studies consistently show that high-quality patient‑centered care is associated with improved clinical safety, treatment adherence, and clinical effectiveness across disease areas and settings.
This article is a guide to notable approaches for enhancing patient outcomes—including why they’re promising, and potential challenges for both clinicians and patients.
6 approaches to improve patient outcomes
Although every specialty and experience is different, the below strategies can all lead to an increase in positive patient outcomes:
1. Patient-centered care
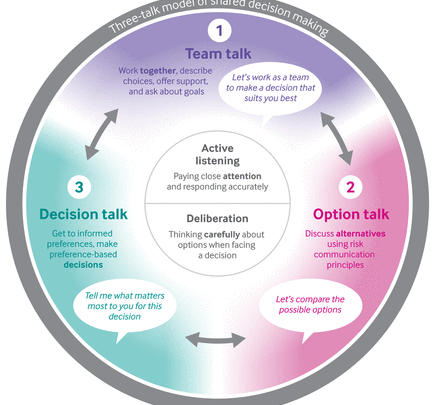
Patient-centered care (PCC) is a clinical model that puts patients’ values, preferences, and life circumstances at the center of medical decision-making. Rather than focusing solely on symptoms or test results, PCC emphasizes treating the whole person—accounting for their social context, goals, and desired level of involvement in care. This approach fosters shared decision-making, empowers patients to participate actively in their treatment, and has been linked to improved health outcomes across specialties.
Researchers conducted a cross-sectional survey of 5,222 hospital inpatients to evaluate patient-centered care’s efficacy. Survey findings indicate PCC significantly correlates with:
- Improving patients’ self-reported physical health
- Enhancing patients’ self-reported mental health
- Increasing patients’ perceived need for hospitalization
PCC frameworks should also address social determinants of health. These include assessing living conditions, education opportunities, employment and other factors that influence health outcomes and perpetuate disparities. Reflecting this, a physician posted on Sermo, writing, “The move towards integrated care systems aims to provide more cohesive services, combining health and social care. This approach can improve patient outcomes and streamline processes.”
2. Patient communication
Quality communication is central to positive patient education outcomes. Almost half (45%) of Sermo community members say that communication is the most important part of the doctor-patient relationship. That’s because when patients understand why they’re being cared for in a certain way, they can build confidence in their treatment.
A growing body of literature demonstrates the effectiveness of certain patient communication methods, including:
- Patient-centered communication: Each patient’s individual needs, preferences, and values guide patient-centered communication. Physicians should let patients speak without interruption, encourage questions, and use plain, easy-to-understand language. This increases treatment adherence and ultimately leads to improved health outcomes.
- Shared medical notes: Offering patients access to their own notes gives them more control over the care process. “Some studies have shown that shared medical notes can help patients to feel more engaged in their healthcare, to understand their medical conditions and care plans better, and to take their medications correctly,” one physician on Sermo wrote. All of these effects can lead to improved outcomes.
- Motivational interviewing: Some physicians use motivational interviewing, or MI, to identify and strengthen patients’ motivations for change. In these conversations, physicians actively listen to identify patients’ unique motivators, ask open questions to surface barriers to change, and collaboratively guide patients toward actionable health goals. Studies show that MI may promote treatment adherence and positive outcomes.
Effective patient communication and evidence-based patient education frameworks, like the teach-back method, work hand-in-hand, leading to improved patient outcomes. Using the teach-back method, physicians ask patients to repeat treatment instructions in their own words. This framework increases patient-centered communication, improving patients’ comprehension of care instructions—especially among those with limited health literacy.
One urologist on Sermo adds, “Every interaction with a patient becomes your opportunity to create a positive experience for the patient. This is especially important when there is a problem, or a patient has a complaint about the service they received in your practice… So, manage your moments of truth. Seize every one of them, even if they are moments of misery, as opportunities to show how good you and your practice are. This will go a long way in building long-term patient loyalty, improving patient satisfaction scores, and may even improve compliance and outcomes.”
Another physician on Sermo says, “Prevention-focused initiatives have significantly impacted my day-to-day work, shifting emphasis from treating illnesses to proactive care. I now prioritize patient education, risk assessments, and preventive screenings. This approach fosters stronger patient relationships and improves outcomes.”
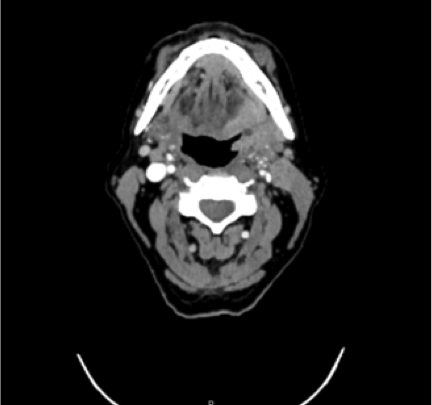
3. Telemedicine
In 2019, the U.S. telehealth market reached $11.23 billion, but COVID-19 accelerated the growth of telemedicine’s adoption by physicians. The market value rose to $17.9 billion in 2020.
Before COVID-19, telehealth accounted for less than 1% of outpatient visits in the United States—limited by inconsistent reimbursement, strict site-of-service rules and interstate licensing barriers. After COVID-19, regulators lifted constraints, insurers expanded coverage and telehealth’s share of outpatient visits rose from 0.3% to nearly 24% at its peak. Physicians and institutions have since continued to adopt telemedicine—its 2024 market value was $35.75 billion.
Physicians in the following specialties have reported notable improvements in patient outcomes by adopting telehealth:
- Cardiology
- Emergency medicine
- Family medicine
- Hematology
- Internal medicine
- Neurology
- Obstetrics and gynecology
- Oncology
- Pediatrics
Across specialties, researchers generally associate telemedicine with improved self-management, better access to care and enhanced continuity of care. More granularly, physicians on Sermo highlight telemedicine’s value for patients managing reduced mobility, transportation limitations or childcare and caregiving responsibilities, among other use cases.
Despite its demonstrated clinical efficacy, telehealth is still a topic of debate among physicians—particularly regarding billing and reimbursement. About 59% of surveyed physicians say telehealth requires the same medical knowledge as in-person visits and should therefore bill at the same rates. The same poll revealed that 34% argued that telehealth is not equivalent to in-person care and should be billed differently.
Contributing to the conversation, one U.S. family medicine physician shared, “Telehealth needs to be thrown away. I cannot believe how many misdiagnoses I have seen when not done in-person. I only use it when the patient is not even in the same state, or defer to an urgent care visit.”

4. Interdisciplinary care
Interdisciplinary care unites physicians across multiple specialties, as well as APPs and other healthcare professionals into a shared treatment model where multiple disciplines assess, plan, and manage care as a team—offering patients a more integrated, safer experience.
Researchers associate interdisciplinary care with various positive patient outcomes, including increased patient safety and reduced medical errors. Here’s why:
- Multidimensional patient assessment: Interdisciplinary care teams combine diverse expertise in patient evaluations. Specialists across disciplines can collaboratively assess physical, psychological, and social factors, identifying details that a single provider might miss.
- Longitudinal care coordination: Care teams often assign a dedicated care coordinator to oversee the continuity across care transitions and facilitate inter-provider communication. This coordination across the care continuum supports smooth transitions and reduces readmission rates by closing communication gaps, educating patients, and maintaining proactive oversight.
- Cross-disciplinary collaboration: Care siloes occur when departments or providers operate independently and without multidisciplinary input. This restricted clinical collaboration can cause diagnostic and medication errors. Interdisciplinary care models break down siloes for more effective, coordinated care.
As examples of patient outcomes, researchers examined 548 hospitals and found that, as cross‐functional team collaboration increased, the percentage of patients who left the emergency department (ED) without being seen decreased. They also indicated that increased collaboration among ED teams shortened the median time patients spent in the ED.
Physicians play a pivotal role in building collaborative care models. By strengthening communication during handoffs, adopting shared tools like SBAR (Situation-Background-Assessment-Recommendation), and actively supporting APP and nursing collaboration, doctors can help dismantle silos and improve outcomes. As Adam Hetz, PA-C and Sermo member, notes, “As a physician assistant, I’ve witnessed firsthand the invaluable contributions that APPs make in filling critical gaps in care delivery.”
5. Quality improvement
While there’s no universal consensus on what “quality” is, quality improvement (QI) generally refers to systems-focused patient outcome solutions. It’s about asking, “Which system changes can lead to better patient outcomes?”
With consistent effort and data-driven adjustments, even small practices can drive meaningful, lasting improvements. Here are strategies that can enhance QI:
- Identify bottlenecks: Locate systemic issues in your practice, whether they’re patient population-specific (like health-literacy barriers) or operational barriers (like inefficient scheduling software). Use internal data (such as from your EHR or patient surveys) and established guidelines, like those from the Agency for Healthcare Research and Quality, to guide your analysis.
- Dive deep: When you encounter issues like long wait times or unsatisfactory communication, consider their root causes. Rather than jumping to conclusions, get second opinions and analyze your process to decide how to move forward. A complete understanding of a systemic problem lets you create meaningful, targeted goals.
- Commit to continuous improvement: Use PDSA cycles to design, test, and refine changes iteratively. This means clearly planning your change with all stakeholders, doing a small-scale test, studying the results, and then acting on insights to refine or scale effectively.
6. Follow-up calls
Following up with patients after appointments and procedures can demonstrate genuine commitment and interest in their care. A U.S.-based dermatologist shares, “Although they [follow-up calls] are time-consuming, they are greatly appreciated by our patients. They simply show you care enough to call them for whatever the reason.”
Follow-up calls aren’t just about good bedside manners—they can improve clinical outcomes. Timely check-ins after appointments or procedures give patients the opportunity to ask clarifying questions, report new symptoms, and receive reinforcement of their care plan. Studies show that post-discharge follow-up is associated with lower readmission rates, better medication adherence, and faster recovery.
An Oncologist on Sermo adds, “Follow-up calls are very important because they generate trust in the doctor-patient relationship and therefore adherence to the therapeutic plan, which is essential to achieve better outcomes.”
While follow-up calls can be time-consuming, they help physicians detect emerging complications earlier, reduce unnecessary ED visits, and strengthen continuity of care—ultimately leading to safer, more effective treatment trajectories.
Learn how other physicians improve patient care
With greater communication and collaboration between physicians, it’s easier than ever to incorporate new methodologies and boost patient outcomes. From telehealth and interdisciplinary care to patient-centered communication and quality improvement methodologies like Lean Six Sigma, multiple proven strategies are helping physicians deliver safer, more effective, and more satisfying care.
Yet, challenges remain. Adoption of these approaches varies, and physician satisfaction with implementation is mixed, underscoring the need for ongoing collaboration, education, and system refinement.
For example, when asked if they were satisfied with the way they incorporated telehealth into their practices, only 42% of surveyed physicians on Sermo said that it was working smoothly, demonstrating a need for improvement.
And on the topic of follow-up calls, a neurologist shares, “Follow-up calls, in my opinion, are fundamental to improve doctor-patient relationship and to better understand the needs of patients. I have always [received] excellent feedback and an improvement in the results of the therapy, in addition to strengthening the empathy and trust of patients.” Insights shared by physicians across specialties in the Sermo community emphasize that continuous learning and peer support are critical for success, and may give you the push you need to improve patient care—and outcomes.
On Sermo, physicians from across the globe discuss the advantages and barriers of evolving patient care models. It’s a space where physicians learn how to improve patient outcomes by leaning on the insights of others. Join the conversation. Become a Sermo member today.