Many physicians, especially when working in hospitals, are assessed by a metric called work relative value units (wRVU), which may determine their pay or bonuses.
Many doctors dislike this metric, and feel it is often used against them. For example, this GP on Sermo says “I would NOT go to wRVU as payment for base pay as it is so easy for an employer to manipulate. Get a base you can live on and have a bonus based on excess wRVU from some set minimum then JUST NEVER expect a bonus since they manipulate wRVU numbers.ˮ
This Sermo member and neurologist also has a low opinion, saying, “At least part of the fault lies in the whole MGMA and wRVU system. MGMA numbers are falsified and exaggerated hugely on wRVU numbers…in Neurology AAN’s carefully studied survey shows the median wRVU of all neurologists is 3700, MGMA says it is about 5300. That is a huge difference. The whole use of MGMA and wRVU must go.”
It is clear that several physicians on Sermo feel that the wRVU system is stacked against physicians, and may interfere with financial planning and predictability. This article will provide an understanding of wRVUs, how they’re calculated, and how they impact physicians.
What are Work Relative Value Units?
wRVUs are the basic component of the Resource-Based Relative Value Scale (RBRVS), which is used to determine physician payment. RVUs measure the value of a service or procedure relative to others, which includes the time a procedure takes, physician expertise (e.g. specialists being paid more than general practitioners), and the resources needed. For example, removing a foreign body from an eye is assigned 0.49 wRVUs, while performing a minor eye wound repair is valued at 1.95, reflecting the fact that about four times as much work is needed to repair the eye wound.
wRVUs don’t directly determine compensation, but RVU counts are mostly used as a way to measure physician productivity. According to an oncologist on Sermo, “RVU counts are generally to make sure everyone is pulling their weight, I.e. You’re bringing in at least what you’re getting paid.”
However, not all RVUs are made equal. One urologist on Sermo explains:
“RVUs are dependent on 3 things:
- Documentation in the office, ED, or hospital (documenting all components for level of service, consult vs. new patient);
- Documenting every component of surgical procedures and being certain that coders submit them. Some uninformed coders do not submit your codes and do not provide feedback;
- How the institution calculating RVUs computes them, e.g., do you add them up or apply 1/2 to the second procedure, 1/4 for the third procedure, etc.
…these variables result in variability when comparing work for different urologists.ˮ
How Work Relative Value Units impact physician compensation
wRVUs are used as a metric to determine how much a physician achieves. Modern metrics look beyond volume, which is an improvement on older systems. The formula is used by Medicare and Medicaid as well as by many medical groups and hospitals.
Physicians earn RVUs based on three components:
- The RVU itself, which is determined by the time taken and a CPT code that reflects the skill and training of the physician (work RVU), the expenses the procedure causes for the practice, and professional liability expenses.
- Geographic practice cost indices (GPCI), which reflect things like the local cost of living for physicians and providers, differences in the cost of clinic buildings, etc.
- A conversion factor that converts the RVU into a dollar amount. The Centers for Medicare and Medicaid (CMS) uses this formula:
(Work RVU* x Work GPCI**) + (PE RVU x PE GPCI) + (MP RVU x MP GPCI) = Total RVU to determine reimbursements.
In this formula, PE stands for practice expense, meaning overhead, non-clinical staff, etc, and MP for malpractice, meaning the cost of professional liability insurance.
The CMS formula given above standardizes physician fees and reduces discrepancies where physicians might be paid very different amounts for performing the same work.The Medical Group Management Association (MGMA) also offers a system many medical groups use, but which physicians tend to think poorly of, and which is not publicly posted – making it opaque to physicians and practices.
For example, one neurologist on Sermo shared their opinion that “MGMA numbers are falsified and exaggerated hugely on wRVU numbers. These large systems (profit and non profit) that use MGMA and wRVU assume that data is true, then turn around and harass, punish and attack physicians for not living up to the highest numbers MGMA can possibly exaggerate to.”
A family doctor on Sermo also says “We have an wRVU bonus and I think it is about 45.00 per RVU. But the threshold to attain it is higher than I care to work.”
wRVUs can be used to determine base pay, but are more often used to set physician bonuses.
wRVU vs. salary-based compensation: pros and cons
Many physicians are on a hybrid model where they are paid a base salary and then receive bonuses based on wRVUs and potentially other measures, such as outcomes. Amongst a small sample of US-based physicians on Sermo, 53% are paid on a hybrid model, 28% a base salary, and 15% solely on wRVUs. These systems for physician compensation have their advantages and disadvantages.
Pros of wRVU include:
- It provides a neutral way to quantify productivity.
- Being paid for a specific unit empowers physicians and helps them feel less like just employees.
- It rewards volume of care and can encourage productivity.
Cons of wRVU:
There are, however, significant cons to consider:
- There is a focus on quantity and not quality. Physicians are rewarded for effort, not patient outcomes.
- The pressure to perform may lead some physicians to “push patients out of the door” and prioritize productivity over providing quality care.
- In the U.S., the CMS controls wRVU values, even for physicians who work for private hospitals. RVU values can go down even as cost of living rises, squeezing physician budgets.
How to calculate Work Relative Value Units (wRVUs)
Many physicians don’t understand how their wRVUs are calculated and paid. 45% of our sample of U.S.-based Sermo users claim they understand their wRVUs well, only 23% understand them very well, and 17% have no idea (the remainder don’t work under this compensation model).
RVUs may be calculated per hour or per visit. When they are calculated per hour, the practice takes the total RVUs a physician generates within a timeline, say a month, then divides them by the hours that physician worked. For example, if a physician’s contract uses a conversion factor of $35 per RVU, and they generate 320 RVUs in a month, they would earn $11,200 for that month. If they worked 160 hours, that equates to $70/hour in effective earnings. Alternatively, if they earned 1 RVU per patient visit, they’d need to complete 320 visits per month (about 16 visits per workday) to earn the same amount.
In the case of a Sermo member and family doctor, “In our system it is about $40 per wRVU, and the average is about 1.15 wRVU per patient. So, 20 x 1.15 = 23 wRVU. 244.5 days = 103.5 wRVU per week. 103.5 x 49 weeks = 5072 wRVU x $40 = $202,860 (gross)ˮ
Other calculations can be more complicated. A pediatrician on Sermo explains:
“In our case, it’s explained that the pay scale is weighted to give compensation to the middle of the curve, and that the higher wRVU levels are lower because you’ve already gotten the benefits earlier. In our plan, there are 7 “steps”. Step zero is base salary at wRVU x $ 34 = salary. Each subsequent step is a range of 500 wRVU, and an addition of base salary.”
wRVUs vary according to industry and location, and may be quite different in, say, Brazil, than at a hospital in the U.S. that takes mostly Medicaid and Medicare payments. Physicians should get as much information as they can about how a specific workplace calculates wRVUs before signing a contract.
Another doctor on Sermo shares how their salary is based on average wRVU: “Every time you see a patient or do a procedure, the code you charge is assigned a RVU value, factors in overhead, time, etc. This is split further to workRVU, your part. Hospitals have data on wRVU production for every specialty, this information is readily available. As a pain doc, wRVU average (50th [percentile]) is around 6000 wRVU per year. That equates to a salary around $480,000. I do around 7500 wRVU annually so naturally everything over that 6000 wRVU threshold is paid as a bonus.”
How to maximize wRVU payments
With wRVUs being so important for physician compensation, many doctors want to maximize the number of wRVUs assigned to them, both to increase earnings and prepare for retirement. Below are actionable steps to do so:
Efficient coding and documentation
Correct coding helps ensure accurate compensation. Doctors should work with coders and billing staff to make sure each visit, procedure, and service is assigned the correct CPT code and properly documented to reflect the level of care provided. Incomplete or vague documentation can lead to undercoding, which directly reduces wRVU totals and thus income. Conversely, upcoding can trigger audits or compliance issues. Consistency in charting, attention to time-based codes, and detailed documentation of medical decision-making all contribute to capturing the full value of a physician’s work.
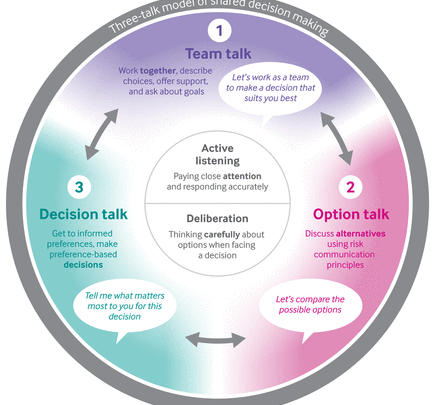
Optimizing patient volume while maintaining quality care
One of the problems with wRVU as a metric is that it can be seen to encourage volume over quality of care. Physicians should endeavor to balance the two. This might mean finding ways to make patient visits shorter, streamlining processes, and working more efficiently – which can be achieved by implementing technological advances, such as increased use of telehealth and/or AI scribes.
Negotiating wRVU-based contracts with fair conversion rates
Physicians faced with wRVU-based contracts should understand what a fair conversion rate is and how it translates to a salary or bonus amount. Conversion rates can vary widely based on specialty, geographic location, practice setting, and payer mix. For example, specialists or physicians in high-demand areas may be able to negotiate higher rates to reflect their market value. It’s essential to review historical wRVU benchmarks, such as those provided by the MGMA or AMGA, and compare them to your expected patient volume and compensation. Physicians should not hesitate to advocate for higher conversion rates, especially if they bring unique expertise, manage high complexity cases, or work in underserved areas. Engaging a healthcare attorney or compensation consultant can also help ensure that contract terms are equitable and sustainable.
Leveraging technology and support staff to improve productivity
Support staff are an important part of productivity. They need to be trained to process patients quickly, reducing the time spent on a visit and increasing the overall efficiency of your practice.
Using modern technology, such as improved electronic health records, can streamline the entire process, reducing wasted time. This also has the pleasant side effect of reducing wait times and appointment delays, improving patient satisfaction.
Join the conversation on Sermo
While the general opinion is that doctors dislike the wRVU metric, many physicians are paid at least in part, on a wRVU metric. Maximizing your earnings by understanding how it is calculated, negotiating the best contract, using technology, and streamlining processes can help you get the most value for your work.
Sermo provides a trusted space for physicians to share real-world experiences with wRVUs, helping peers uncover system flaws, benchmark more accurately, and negotiate better contracts through community-driven insights.