The Centers for Disease Control and Prevention (CDC)
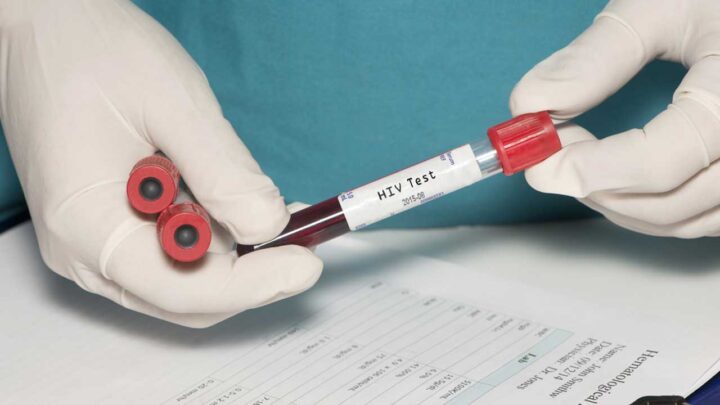
Point-of-care HIV tests and over-the-counter self-tests have helped broaden the reach of HIV testing, leading to a steady increase in the proportion of estimated people with HIV who know their status. However, there is more to be done to end the HIV epidemic by 2030 – a goal of the HHS Ending the Epidemic in the U.S. initiative. Following are three key HIV screening statistics that every health care provider should know in their critical role to screen all patients.
An Estimated 1 in 8 People with HIV Don’t Know They Have the Virus.
Approximately 158,500 people with HIV in the United States remain undiagnosed and are not benefiting from early diagnosis and antiretroviral treatment. To address this critical gap, the Centers for Disease Control and Prevention (CDC) recommends everyone between the ages of 13 and 64 get tested for HIV at least once as part of routine health care and that those with ongoing risk be screened at least annually. By making opt-out HIV screening the standard of care in your practice, you can help to reduce HIV transmission for all your patients. Adopting an opt-out approach is as simple as informing your patients through a patient brochure, practice literature/form, or discussion that an HIV test will be included as a standard preventive screening test and that they may decline the test. You can start the conversation with your patients by telling them that HIV testing is a routine part of health care, just like getting their blood pressure checked.
75% of People at Increased Risk for HIV Are Not Getting Tested Every Year.
Despite seeing a primary care provider, approximately 75% of people at increased risk for HIV are not getting tested every year, including heterosexual people at increased risk, people who inject drugs, and men who have sex with men. HIV crosses the boundaries of gender, sexual orientation, age, race, and ethnicity. You can ensure equitable care in your practice by offering HIV screening to all your patients. Many health care providers integrate routine HIV screening into their practice by telling patients, “I perform a one-time routine screening for HIV for all patients,” to help normalize the test.
After administering an HIV test, implement a status-neutral approach by linking your patients with a positive test result to HIV treatment services and connecting patients who test negative with prevention tools, such as pre-exposure prophylaxis (PrEP) and condoms. By providing HIV services to all patients, whether they test positive or negative, we can work toward a future without HIV.
1 in 5 People Who Receive an HIV Diagnosis Already Have the Most Advanced Stage of the Disease.
By screening all patients for HIV, you can connect those with a positive test result to medical care, including antiretroviral therapy (ART) and other services, as quickly as possible. CDC recommends that people start treatment as soon as possible after diagnosis to gain maximum benefit from ART. ART reduces HIV-related morbidity and mortality at all stages of HIV infection, and people with HIV who take ART as prescribed and achieve and maintain an undetectable viral load have effectively no risk of transmitting HIV through sex. This is known as treatment as prevention or Undetectable = Untransmittable (U=U).
CDC Offers Free HIV Screening Resources.
Any clinician looking to get started with routine HIV screening or brush up on their current skills can explore CDC’s new suite of HIV screening materials, including patient and provider brochures and posters for your practice. The Screen for HIV Toolkit is one in a set of three new toolkits designed to inform the future of HIV screening, prevention, and treatment.
Here is more of what some HCPs have to say on routine HIV screening as the standard of care.
While it may be unfamiliar territory to some, there are several key strategies and conversation starters that any clinician or nurse practitioner can easily adopt to integrate HIV screening into their routine clinical practice.
Jason Farley, PhD, MSN, MPH, RN, ANP-BC, FAAN, FAANP, AACRN
As a primary care provider, it feels so impactful to be first touchpoint for HIV testing and linkage to care.
Dr. Sampath Wijesinghe, DHSc, MS, MPAS, PA-C, CPAAPA, AAHIVS
Clinicians can help reduce HIV infections by 90% by 2030 if we make a commitment to screen for HIV, prescribe PrEP, and link patients to treatment and care.”
Dr. Michael Saag, MD
Everyday thousands of Sermo member physicians from diverse backgrounds and experiences exchange knowledge with each other. Sermo is the original medical social network that empowers today’s physicians. Over 1 million fully verified physicians across more than 150 countries come to our platform to talk with peers, participate in paid medical studies, solve challenging patient cases, contribute to the world’s largest database of drug ratings – and enjoy a few laughs along the way.
Interested in more? Check back any time and follow us on Facebook, Twitter, and LinkedIn for the latest and greatest in physician insights.