Every year, the CDC’s Advisory Committee on Immunization Practices (ACIP) sets the tone for vaccine guidance in the U.S., influencing everything from patient conversations to payer policies to public health campaigns. When the ACIP met in September 2025, it rolled out a new set of recommendations that immediately sparked conversation across the healthcare community.
The updates covered a wide range of issues, from COVID-19 vaccine eligibility to childhood immunization schedules. For many clinicians, these recommendations provide much-needed direction. For others, they raise more questions than answers.
To capture the pulse of frontline providers, Sermo surveyed 243 of our triple-verified healthcare professionals – including US PCPs, pharmacists, pediatricians, OB/GYNs and NP/PAs. Their responses reveal both confidence and concern, especially when it comes to COVID-19.
Clarity vs. confusion
On the surface, most providers said they could make sense of the new recommendations. A combined 75% described the guidance as very or somewhat clear.
But that still leaves one in four clinicians who struggled with interpretation—an important signal when guidance is meant to drive consistent practice. Pediatricians stood out in particular: more than half reported confusion, with one in five describing the recommendations as very confusing.
When asked where the uncertainty lay, three areas rose to the top:
- COVID-19 (77%)
- MMR/Varicella (58%)
- HepB (55%)
This suggests that even with ongoing updates, the messaging around vaccines, especially in pediatrics, isn’t always translating smoothly into clinical workflows.
Agreement with the decisions
Clarity is one thing. Agreement is another.
Overall, a majority supported the ACIP’s decisions, with 29% strongly agreeing and 43% somewhat agreeing. But the data tells a more nuanced story when broken down by specialty.
- Pediatricians were more skeptical, with nearly 70% disagreeing to some degree.
- Nurse practitioners, on the other hand, were far more supportive, with nearly half strongly agreeing with the outcomes.
These differences highlight how practice setting and patient population shape the way national recommendations are received—and ultimately, how they’re implemented.
COVID-19 guidance: evidence, access, and conversations
COVID-19 continues to be the lightning rod.
When asked if the new recommendations were grounded in real-world clinical evidence, six in ten said yes. However, that figure drops to 46% among physicians only, leaving a sizable portion of providers cautious about the data backing.
Access was another hot topic. Providers strongly favored federal guidelines (63%) over state-by-state decision-making, signaling a clear desire for national consistency.
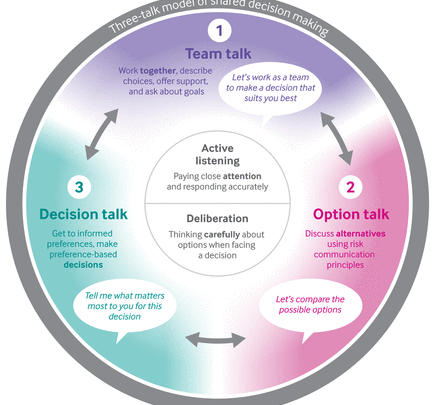
The recommendation for shared decision-making proved especially divisive. Nearly half of clinicians (47%) said this approach would make conversations with patients harder. That sentiment was even stronger among specialists, rising to 68% of OB-GYNs and 74% of pediatricians. Only 29% of clinicians overall felt it would make conversations easier, while the rest anticipated no change. For many, the added nuance may complicate discussions rather than clarify them.
When it comes to prescribing authority, most providers wanted physicians to remain central (90%). But there was also strong support for nurse practitioners (84%) and physician assistants (77%), with two-thirds backing pharmacists as prescribers. The consensus? Broader access matters.
As for which groups should be prioritized under the new guidance, providers pointed to those at highest risk:
- Adults 65+ (88%)
- Immunocompromised patients (86%)
- Pregnant women (54%), though OB-GYNs stood out, with 81% saying they would recommend vaccination for this group
- Healthy adults (42%)
- Healthy children (40%)
This paints a picture of clinicians weighing risk-benefit carefully, with the most enthusiasm reserved for high-risk populations.
Beyond COVID-19: childhood vaccines and public concerns
The ACIP also updated its recommendations for childhood vaccines, including guidance that children under age 4 receive separate MMR and varicella shots instead of the combined MMRV vaccine. On this, providers were split: 60% agreed, 40% disagreed.
The bottom line
The September 2025 ACIP meeting clearly left an impression. While most clinicians support the committee’s decisions, not all are convinced by the clarity or the evidence base, and specialties diverge sharply in their interpretation.
For pediatricians, confusion and disagreement stand out. For nurse practitioners, agreement is stronger. And across the board, COVID-19 continues to dominate discussions, raising questions about evidence, communication strategies, and access.
Looking ahead, consistency and transparency will be key. Providers want clear guidance that they can easily translate into patient conversations without ambiguity or mixed messaging.
At Sermo, we’ll continue amplifying these frontline perspectives. Because when it comes to public health policy, the people delivering care deserve to have their voices heard.