An estimated 1.6% of the adult population in the United States are transgender or nonbinary, according to a 2022 Pew Research survey, with the majority of the share in adults younger than 30. This highlights the need for competent gender-affirming healthcare to meet the needs of the next generation of patients.
Many physicians would like to see more focus around communication strategies and clinical protocols that best serve this population. In a poll of physicians on Sermo, only 35% said they feel there is enough support for gender-affirming care. This guide explores the essential components of gender-affirming care, drawing from peer-reviewed research, clinical guidelines and real-world insights from practicing physicians worldwide.
What is gender-affirming care?
Gender-affirming care encompasses a broad, evidence-based approach that includes medical, psychological and social support aligned with a patient’s gender identity. This framework addresses the needs of transgender and gender-diverse individuals through multiple intervention pathways.
The clinical components of gender-affirming practices include hormone therapy for trans patients, such as estrogen or testosterone replacement, puberty blockers for adolescents experiencing gender dysphoria, and various surgical interventions when appropriate. Gender-affirming care also includes counselling, with ongoing therapeutic relationships that support patients throughout their journey.
According to Sermo community data, physician engagement with gender-affirming care varies. When asked whether they provide gender-affirming care for patients, 37% of respondents said yes, 29% said no, 16% said sometimes depending on the situation, and 17% said it wasn’t applicable to their specialty. “While I strive to offer support and resources whenever possible, my ability to provide this care may depend on the specific circumstances, including the resources available in my practice or specialty,” writes one pathologist.
Regional gaps play a part in availability. 39% of surveyed physicians indicated that gender affirming care is available in their region, while 28% said yes – but with restrictions and wait lists. In the poll, half of respondents said surgical and medical services are available in their area, while others voted:
- 14% said medical transitions such as HRT are available
- 4% said surgical transition services can be accessed
- 9% said no gender-affirming care is available in their region whatsoever
- And 22% weren’t sure.
Why gender-affirming care saves lives
The mental health benefits of gender-affirming care extend far beyond immediate psychological relief, creating lasting improvements in quality of life. A 2022 study found that access to gender-affirming hormone therapy was associated with lower odds of recent depression and suicide attempts among transgender and nonbinary youth.
Sermo members have emphasized this connection. “The fact that gender change is allowed in many countries has allowed the suicide rate to decrease, as it helps people who do not identify with their gender to have a better quality of life and feel better about their bodies. It is a step forward in our society,” writes one general practitioner on Sermo.
A family medicine physician from Brazil also weighed in. “Gender-affirming care is essential to the health of transgender individuals, improving their mental well-being and reducing the risks of depression and suicide,” they write. “Medical organizations such as the AMA and APA support this care as needed, not optional.”
The clinical evidence supporting gender-affirming practices extends beyond mental health outcomes. It may lead to improved treatment adherence in some instances. When patients trust their healthcare providers and feel respected in clinical settings, they are more likely to maintain ongoing relationships with the healthcare system.
Research suggests gender-affirming care can improve patients’ psychosocial functioning. Healthcare providers who have witnessed the effects firsthand understand the profound impact of affirming care. “After being a medical student participating in a transition surgery, I realized how life changing it could be for patients,” writes a U.S.-based psychiatrist on Sermo.
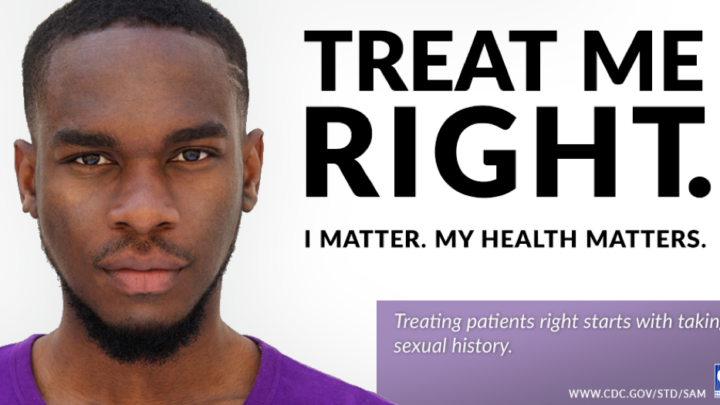
How physicians can communicate with respect and empathy
Gender-affirming care requires intentional strategies that prioritize respect, empathy and clinical sensitivity. A welcoming environment encompasses thoughtful language choices and every other aspect of the patient encounter.
Inclusive language avoids assumptions about gender identity based on appearance, voice or legal documents. Instead of defaulting to binary pronouns, healthcare providers can model inclusive communication by introducing themselves with their own pronouns and asking patients about their preferred pronouns respectfully. During clinical encounters, asking open-ended questions about health concerns allows patients to share information about their bodies and experiences using their own terminology.
A family medicine physician on Sermo admits that they sometimes fall short. “When I see a person for the first time, I try not to assume my patients’ gender from their external appearance and their first name, and therefore address them in as neutral a language as possible, but I must admit that it is difficult and I often fall into the trap of addressing them as if I have deduced their gender sense from their clothing, accessories, hairstyle, presence or absence of makeup, behavior and name,” they write. When mistakes occur—and they inevitably do during the learning process—swift acknowledgment and correction demonstrate respect for patients’ identities.
Other ways to create a welcoming environment include updating intake forms to include diverse gender identity options, training front desk staff on respectful communication, and displaying inclusive materials in waiting areas. These cues signal to patients that the practice is prepared to provide affirming care.
Confidentiality takes on additional importance in transgender healthcare, as patients may not be “out” to family members, or may face safety concerns if their gender identity is disclosed without permission. Many transgender individuals avoid disclosing their gender identity publicly due to fears of stigma, discrimination, harassment, or violence from family, community, or even within healthcare settings. Some may have experienced or fear denying care, disrespect, or even physical assault when their identity is known. Others may avoid disclosure due to lack of support, or because they come from unsupportive or abusive family environments where disclosure could lead to rejection, abuse, or homelessness. Additionally, the environment of the healthcare setting itself—such as lack of privacy or risk of being misgendered or outed by staff—can dissuade patients from being open about their gender identity.
Clear discussions about confidentiality boundaries help build trust and ensure patient safety.
How to provide the best gender-affirming care possible
The optimal approach to gender-affirming care can vary based on patient age, health status, personal goals and available resources.
For adolescent patients, puberty blockers represent a reversible intervention that can provide time for psychological development and decision-making. These medications temporarily pause puberty-related changes that may cause distress, allowing young people and their families to explore gender identity without the pressure of irreversible physical changes. During treatment, physicians should monitor growth and bone mineral density to avoid potential long-term complications.
Gender-affirming hormone therapy is available to adult patients, but requires careful medical oversight. Testosterone therapy for transgender men typically involves intramuscular injections or topical preparations, while estrogen therapy for transgender women may include oral, transdermal or injectable formulations. Before initiating hormone therapy, baseline assessments such as liver function tests, lipid profiles, hematocrit, and hormone levels are recommended. Ongoing monitoring during treatment is essential to assess hormone levels, blood pressure, and potential adverse effects like thromboembolism risk with estrogen or polycythemia with testosterone, with dosing adjusted accordingly.
Routine screening protocols require thoughtful adaptation for transgender patients. Cervical cancer screening remains necessary for transgender men who have not had hysterectomies, while breast cancer screening applies to transgender women receiving estrogen therapy. Prostate cancer screening continues to be relevant for transgender women, regardless of hormone use.
A family medicine physician highlights the importance of an individualized approach on Sermo. “Gender-affirming care is not a one-size-fits-all approach and different trans and nonbinary people may have different needs and preferences, the most important thing is that each person has the autonomy and agency to decide what is best for them and that they receive respectful and competent care from whoever is providing it,” they write.
Navigating barriers to gender-affirming care
Healthcare providers and patients face numerous systemic challenges in accessing and delivering gender-affirming healthcare. Restrictive policies at state, national and institutional levels can limit the types of gender-affirming practices available to patients. When polled on whether their country or state has policies about gender-affirming care, 47% of Sermo members said yes, 23% said no, and 30% were unsure.
Accessibility represents a significant barrier, particularly in rural or underserved areas, thus many patients must travel long distances or face extended waiting periods for appointments. This creates additional stress and financial burden for patients seeking care.
Patients can face significant financial barriers, such as loss of income from time off work, travel expenses and associated medical testing. Insurance coverage remains inconsistent across different regions and insurance types. While some plans have expanded coverage for gender dysphoria treatment, others continue to exclude transgender-related services or create administrative barriers through prior authorization requirements and limited provider networks.
A general practitioner on Sermo points to education gaps as a key barrier. “I think that even more information is needed to improve the way the medical community provides gender-affirming care and thus know even more how to refer to patients, we have to know what type of pronouns exist and what is the pronoun with which our patient feels more comfortable,” they write.

What physicians are saying on Sermo
The Sermo community provides insights into how healthcare providers worldwide approach gender-affirming care.
A general practitioner from Pakistan underscores the holistic scope of gender-affirming practices. “It’s a whole-person approach that can include things like hormone therapy to help their bodies match their gender identity, surgery to make physical changes, counseling and therapy to support their mental health, and regular healthcare that’s sensitive to their needs, like sexual health check-ups and preventative care,” they write. “Plus, they get social support too, like help with legal name changes, documentation, and navigating social and workplace challenges.”
An ophthalmologist from Brazil emphasizes the psychological benefits. “I believe that gender change helps in self-acceptance, freedom of expression and decreased suicide rate,” they write. A cardiologist from Cuba sees value in the facets of gender-affirming care. “If you wish to medically transition with hormones or surgery, specialized care is required to avoid problems,” they write.
An ophthalmologist from Canada urges fellow practitioners not to remain dismissive. “We are still learning about this and [the] medical field need[s] to have open views on this and not be so quick to just pass it off as [a] mental disorder as I can see in the comments some mention this.”
The community discussions on Sermo reveal healthcare providers grappling with complex ethical, clinical and social questions. These peer-to-peer exchanges contribute to collective learning and improved clinical practices across healthcare settings.
Building competent and compassionate care
The evolution of gender-affirming healthcare reflects broader trends toward personalized medicine, patient autonomy and evidence-based practice. The integration of gender-affirming care into routine medical practice benefits patients by promoting inclusive environments, respectful communication and individualized treatment approaches. These skills can transfer across all patient populations, enhancing overall care quality and patient satisfaction.
The medical community’s growing engagement with transgender healthcare issues demonstrates the profession’s commitment to serving all patients with dignity and respect. As one GP shares, “the Hippocratic Oath i swore mandates me to give care to all irrespective of religion, creed, culture, sex or whatever affiliations. That’s my guiding principles.” Through platforms like Sermo, healthcare providers continue to share insights, ask questions and collaborate on best practices that make medicine more inclusive.
Join the conversation on Sermo to connect with colleagues who are passionate about providing excellent patient care across all populations. Our community regularly shares clinical insights and evidence-based strategies to help fellow healthcare providers deliver the highest quality care possible.