Gone are the days when patients had to be physically present for their physicians to capture their health data. Remote patient monitoring (RPM) allows physicians to monitor their patients’ stats through digital devices. From diabetes to respiratory illness, RPM is reshaping how physicians monitor, engage and care for patients across specialties.
Remote patient monitoring does not replace routine in-person monitoring, but rather supplements it. “Remote monitoring and in-person monitoring play important roles in healthcare, each with their own strengths and weaknesses, the choice of the appropriate method will depend on the specific needs and condition of each patient, as well as the resources and technology available,” explains a GP on Sermo. “In the healthcare environment, in many cases, a combination of both approaches can provide comprehensive and effective care for patients.ˮ
Continuous monitoring not only provides ongoing health data that allows for better adjustment of treatments, but can also be used to empower patients and give them more control over their own care. This article explores the evolving role of RPM in healthcare today.
What is remote patient monitoring (RPM)?
Remote patient monitoring is the use of technology to capture health data from patients outside of the clinic and transmit the data to healthcare providers. RPM systems may also provide the data directly to the patient. For example, smart glucose monitors provide both the provider and the patient with ongoing blood sugar data that the doctor can use to monitor the patient, and the patient can use to adjust their diet accordingly and in real time.
RPM became prevalent during the COVID-19 pandemic when many patients with chronic illnesses were afraid to go to the doctor. Although the pandemic is over, RPM is still commonly used. “Telemedicine and remote monitoring are here to stay,” writes one family medicine doctor on Sermo. “It is a useful tool that saves travel by both the professional and the patient, which leads to better control at a lower cost.ˮ
When asked what they think is RPM’s most significant benefit, 47% of physicians on Sermo highlighted that they help improve management of chronic conditions. “Remote monitoring of patients is a very effective tool for the control of chronic diseases; it helps improve therapeutic adherence and is also a way to improve accessibility to health services, reducing costs in care and expenses for patients and families,ˮ writes one infectious disease specialist.

Most common use cases of RPM
RPM can be used for a variety of conditions. Here are some of the most common:
Chronic disease management
RPM is useful for chronic disease management, particularly diabetes, hypertension and heart disease. Smart glucose monitors and blood pressure monitors are amongst the most common RPM devices physicians and patients use.
Blood pressure is particularly important as some people experience anxiety in a doctor’s office, artificially raising numbers. “There are different remote monitoring methods that we use in our practice such as ABPM and Holter for blood pressure,” says a nephrologist on Sermo. A GP from the UK shared that they “offer remote monitoring for BP monitoring, blood glucose monitoring,” and “give the monitoring supplies in cases where the patient cannot afford to purchase [their] supplies themselves.”
However, one family doctor on Sermo holds the opinion that “short-term monitoring for a specific observation is best use. Cardiac, glucose and sleep apnea breathing patterns come to mind. Longer-term continuous monitoring would cost the same as a person moving in with the patient and monitoring them in-person.”
Post-surgical care and recovery monitoring
Some physicians use remote monitoring for patients recovering from surgery to reduce their number of post-operative visits and identify complications faster. This can include tracking wound healing via secure photo uploads, monitoring vital signs for early signs of infection, and collecting patient-reported pain or mobility data. By identifying issues sooner, doctors can intervene before complications escalate, potentially reducing readmissions and improving patient comfort during recovery at home.
Elderly and at-home patient care
RPM can play a part in elderly and at-home patient care. It shows a lot of promise for reducing hospital admissions, particularly in older patients who have more than one chronic condition. Fall monitors, heart monitors and blood pressure monitors can all contribute to helping people stay home longer and lead a more independent life.
Infectious disease monitoring
Remote monitoring can reduce the need for physical proximity with patients diagnosed with an infectious disease, lowering risks for spreading disease while still allowing for quality care.This is especially important for vulnerable populations like the elderly, immunocompromised, or chronically ill patients.
Benefits of remote patient monitoring
Remote monitoring technology has a variety of benefits for both physicians and their patients. Here are some key benefits to consider:
Benefits for physicians
Physicians can use tools, including AI, to continuously monitor data in real time. This allows them to respond to problems before they become crises, and make decisions about medication dosage and treatment protocols in real time if needed. This also allows physicians to use their time and resources more efficiently, leaving more time for patients who require immediate in-person care.
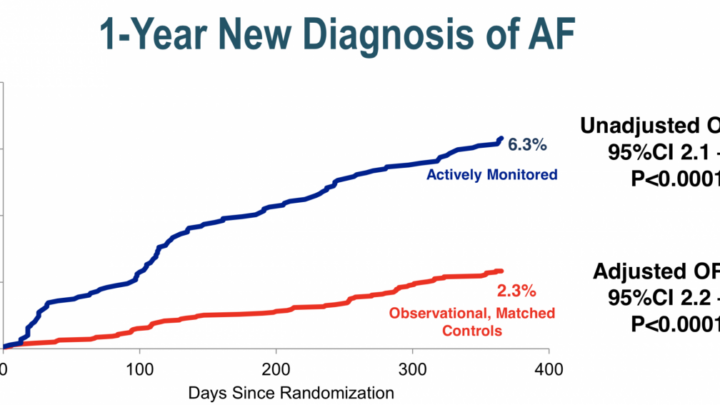
“The advantages of remote monitoring for diseases, mainly cardiac, are undeniable,” writes a neurosurgeon on Sermo. “Recording what happened and reading it at the desired time is part of the ease of work it offers.ˮ
RPM improves communication between physicians and patients and increases patient adherence. Family caregivers can become more involved and are more likely to collaborate with physicians, reducing conflict and improving care.The downstream effects include reduced risk of hospital readmissions and emergency visits, which contribute to reduced costs for practices and hospital systems.
Benefits for patients
The two primary benefits for patients are:
Increased convenience: Patients and caregivers have to make fewer trips to an office or clinic, saving time and potentially money. Home-based monitoring is also typically more comfortable and allows for more flexibility as it fits into the patient’s daily routines.
Increased involvement: By becoming an active participant in their care, patients are better able to manage their condition as they must learn how to interpret their results, and the treatment plan can be adjusted as needed. Research shows that patients who are better educated about their conditions have better outcomes, lead a better quality of life, and can manage their conditions more effectively.
“In my opinion, telemonitoring improves care for patients with heart problems,” says a GP on Sermo. “It enables them to keep a close eye on their state of health at all times, and to forge a therapeutic alliance.ˮ

Challenges of remote patient monitoring
RPM is relatively new technology with three key challenges that need to be addressed:
Data security and patient privacy concerns
Transmitting patient data over the internet brings obvious security and privacy concerns. Systems used must meet privacy requirements such as those laid out in HIPAA in the United States and GDPR in Europe. Data encryption is a requirement.
Healthcare providers are commonly victims of cyberattacks. In 2024, 736 healthcare data breaches affecting 500 or more people occurred in the U.S. alone. With that fact in mind, it is clear why physicians on Sermo view cybersecurity as a major concern. In one survey on the use of RPM in managing heart conditions, 51% of respondents felt data security was a barrier they faced.
Physicians can address and prepare for these concerns by:
- Utilizing the services of cybersecurity experts and IT professionals to conduct regular security testing on systems in use.
- Educating both staff and patients on safe device use, password security, and awareness of common phishing attacks or data breach concerns.
- Ensuring that their practices have clear protocols in place for what to do if they believe data has been compromised.
Technology accessibility and digital literacy issues
RPM brings up accessibility concerns. 74% of physicians polled on Sermo express a concern that remote monitoring could contribute to healthcare disparities due to the digital divide. “A potential exclusion is the limited access to technology or reliable internet connectivity, especially in rural or underserved areas. This can hinder the adoption of remote monitoring, as patients may not have the necessary devices or infrastructure to participate effectively,ˮ says one ophthalmologist on Sermo.
The patients that benefit from telehealth and remote monitoring the most are the ones with the biggest challenges accessing it – patients in rural areas. Rural broadband is of low quality in many areas, including parts of the U.S., and inclement weather can result in temporary loss of real-time data. Physicians can improve access for rural populations by discussing and identifying potential challenges with patients before prescribing RPM, and advocating for policies that expand reliable internet access to all Americans.
51% of polled physicians on Sermo said that the biggest barrier they faced was patient access or comfort with technology. Older patients in particular may lack digital literacy. This means that doctors may need to help these patients to learn how to use monitoring equipment properly as incorrect use can sometimes lead to inaccurate data. This can be achieved by sharing educational resources such as how-to guides, or selecting devices with intuitive user interfaces and minimal setup.
Regulatory and reimbursement challenges
Since RPM is so new, insurance companies may be reluctant to cover the costs to patients. While Medicare and Medicaid cover RPM, it’s only in certain cases. There is often little consensus as to who should pay for devices. In some cases, remote monitoring devices may be indistinguishable from consumer-grade “health wearables” and this could put the cost burden onto patients. Physicians can assist patients by documenting the clinical relevance of these devices for insurers and staying up to date with RPM billing codes.
36% of polled US-based physicians on Sermo felt this was the biggest barrier towards adoption. While RPM may reduce costs to patients, this is only helpful if any up front costs are in reach. Practitioners can use these lower long-term costs to make a case for insurance coverage, but this may or may not be successful. Exploring grant options, trial devices, and partnerships with device manufacturers for discounted rates can also be an option.
How physicians can implement remote monitoring
Physicians and practices that choose to implement remote patient monitoring should follow these steps:
- Set up systems that support it. This includes integrating the data into electronic health record (EHR) and healthcare information exchange systems and exploring the use of consumer-grade wearables patients may already own. Identify the conditions you want to monitor remotely and how this data will be accessed.
- Identify patients who are eligible for RPM and have the potential to benefit from it.
- Determine insurance or Medicare/Medicaid coverage. Explore costs and alternative funding options that could be suggested to patients if insurance coverage is not guaranteed.
- Obtain consent from the patient and educate them on the benefits of the system so they are more likely to comply with its use.
- Order or prescribe the RPM. Ensure that the patient or primary caregiver is able to use the equipment, and allow them to take the device home.
- Obtain the data from the device, analyze it, and make it available to the patient and/or caregiver if applicable.
- Give guidance to the patient based on the results.
- Provide ongoing support for technical problems and assistance on how to properly use the device(s).
The takeaway
RPM is a tool that is becoming more and more available and is especially useful for those dealing with chronic health conditions with complex treatment plans. By lowering costs and empowering patients it improves treatment adherence and supports higher quality outcomes.
Sermo offers a unique opportunity to discuss the challenges and opportunities associated with RPM and other emerging medical technologies. Join today to collaborate with thousands of your peers on a variety of trends and important clinical topics.