Advances in cancer treatments have increased the number of cancers treated using immunotherapy. The percentage of patients selected for immune checkpoint inhibitor drugs – a subtype of immunotherapy – has increased from 1.54% in 2011 to 43.63% in 20181. The percentage response of patients to immune checkpoint inhibitor drugs increased from 0.14% to 12.46%. With selection increasing 29 times and response surging by 89 times, immunotherapy is quickly becoming mainstream for cancer patients.
Cancer immunotherapy offers an additional layer of hope to cancer patients, but some oncologists face a daunting task managing patients’ optimism and the realities surrounding these evolving immune system therapies. This article explores common patient misconceptions about immunotherapy, and looks at how oncologists can be both realistic and hopeful when managing patients who are either inquiring about immunotherapy or who may actually be candidates for it.

Two major immunotherapy misconceptions
The news and social media typically report immunotherapy clinical trial breakthroughs, but the media typically does not reveal the full picture of novel efficacious immunotherapy drugs. These information gaps could lead cancer patients to have unrealistic expectations about immunotherapy. Here are two major misconceptions surrounding immune system therapy that many patients have:
1. Immunotherapy cures every type of cancer
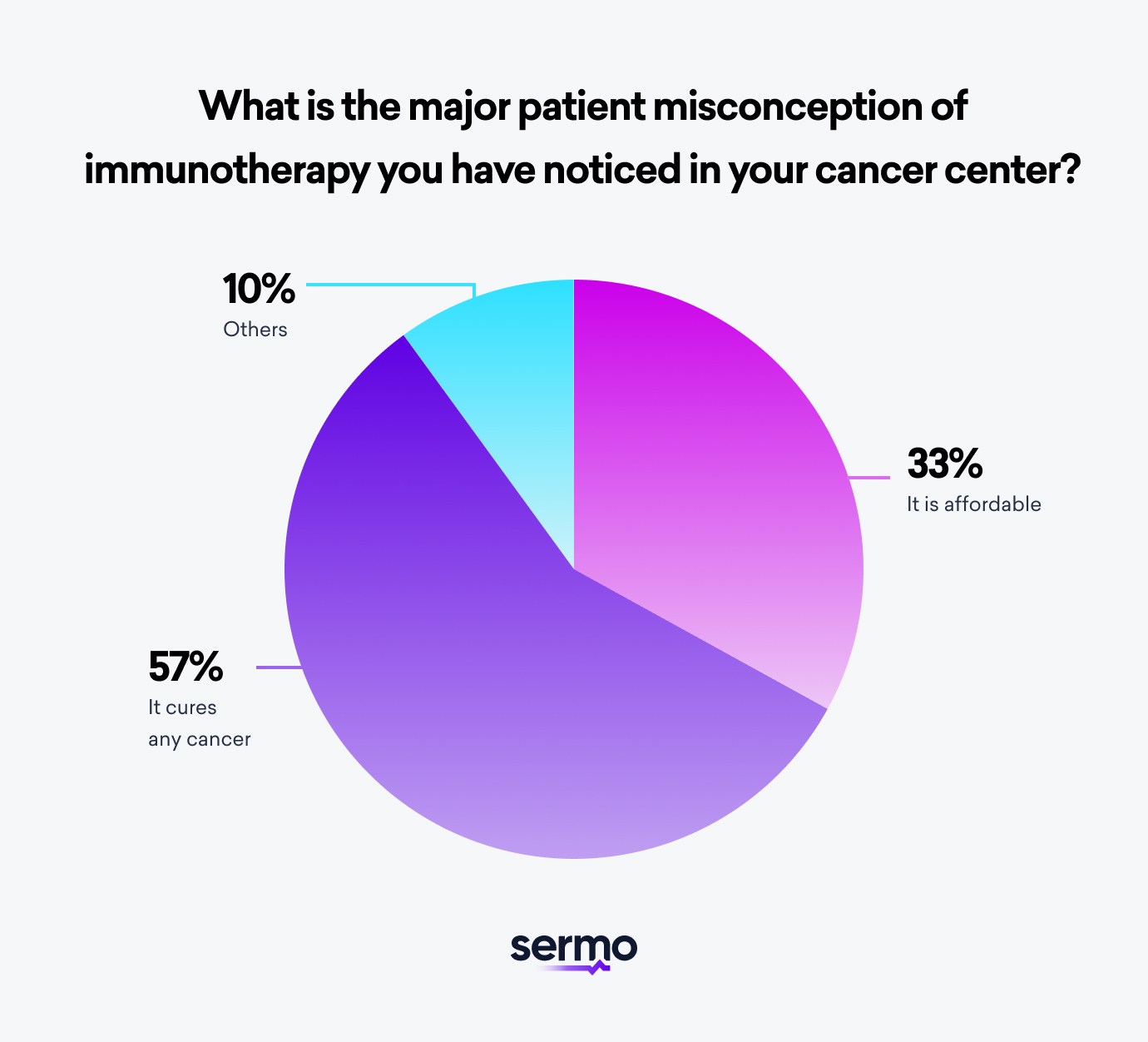
In a 2022 Sermo survey of specialists in our community, 56% of these experts reported that most patients wrongly believe that immunotherapy cures any type of cancer. This misunderstanding could be due to media headlines on the latest cancer immunotherapy drugs that give patients false hopes.
Some cancer patients may discuss these cancer therapy discoveries with their oncologist with the hopes of getting treated with a new immune system drug. These patients are typically unaware that the apparently effective new immunotherapy drugs may not be suitable for their immune responses and specific innate immunity.
“Patients believe immunotherapy can cure cancer into remission and it is safer than chemotherapy with little to no side effects. They also think it can be given at any time, even to every sick patient in the ICU”. A pulmonologist in the Sermo physician community stated in one of our recent surveys.
These patients have these misconceptions because they do not have sufficient medical information to alter their beliefs. Many patients do not consider other indications for selecting an immunotherapy intervention. For instance, an immunotherapy drug may have a potentially life-threatening adverse effect that could make it unfit for a patient.
According to recent immune system studies, inhibitory and stimulatory tumor checkpoint expression levels are likely not the only factors underlying immunotherapy difficulty and resistance. Oncologists and researchers should consider the tumor microenvironment (TME) landscape in greater depth from the aspect of immune cells in addition to the tumor histology, molecular subtype, clonal heterogeneity and tumor cells evolution as well as micro-changes in the fine structural features of the tumor area and infected cells.
New research exposes how the immune system protects us against cancer cells. Several immune cell populations, including activated CD8 T cells, b cells signatures, natural killer cells, and CD4 helper 1 T cells, are associated with favorable patient prognosis. In contrast, other immune cell populations, including myeloid-derived suppressor cells, regulatory T cells, and tumor-associated macrophages, are involved in immune checkpoint inhibitors and tumor immune escape. These suppress immune responses and are associated with worse patient prognosis.
Therefore, it is critical for oncologists to inform their patients by educating them on the potential risks and limitations of immunotherapy. Oncologists may even dive into the study details that were not published in the media report and explain grey areas clearly. And further, explaining why the preferred conventional treatment may be a better option could also strengthen the doctor-patient relationship and position the physician as being open to different approaches but still ultimately wanting the best option available for a patient’s unique case.
2. Immunotherapy is affordable
Some patients may believe new immunotherapy drugs are affordable and/or covered by insurance. These cancer patients may not understand the degree of financial burden novel cancer treatments entail. In some cases, the average price of a newly launched cancer drug can exceed $100,000 per treatment course2 per patient. These high costs do not guarantee a positive immune system response, activation of lymph nodes and white blood cells, or even to effectively destroy cancer cells.
Also, the average age for cancer diagnosis in the United States is 663 years, and the US Census Bureau data reports that the average mean retirement income for retirees aged 65 years and above is $73,228. These figures suggest that it will be a heavy burden for the average US retiree to afford cancer treatments.
Hence, it is vital for oncologists to explain these realities to patients, even if they are eligible for cancer immunotherapy. Patients need to clearly understand the financial commitments and potential negative side effects involved before treatment commences.

How oncologists can manage patient immunotherapy expectations
Oncologists typically encounter patients at various levels of awareness about cancer immunotherapy. Some patients are new to immunotherapy and require more counseling. Others are knowledgeable but need guidance with information gaps. Here are some strategies oncologists can use to manage cancer patients’ immunotherapy expectations.
Provide optimistic and realistic counsel
Educating your patients about specific clinical details of immunotherapy will help them make better decisions. With a sense of hope after several failed chemotherapy treatments, some patients choose immunotherapy without due consideration. It’s helpful to cover the basics of how the immune system works to produce antibodies in order to fight cancer in addition to the typical immune response to fight infectious diseases. Include a brief overview of stem cells, t lymphocytes, b lymphocytes, memory cells, and the difference between normal cells and abnormal cells. Do not get overly medical, but when you this context about the adaptive immune system and lymphatic system your patients will be better prepared to discuss treatment options and outcomes.
It is necessary for oncologists to discuss the risks and limitations of immunotherapy as well as other cancer treatments available. Physicians can explain the role of genomic testing and meeting eligibility criteria for different types of cancer when determining an individual’s suitability for immunotherapy. You can educate your cancer patients on the treatment realities while staying optimistic. Empowering your patients with all the relevant details and immunotherapy facts helps them make a shared decision that could positively impact their health outcome.
Access to updated online resources
As a physician, you don’t have to do all of the educating in person. Most cancer centers have a website where patients can access quality information about cancer care and their services. Referring them to these sites and other factual research may empower them to learn more. Further, according to a respiratory physician in our community, “The new treatments based on immunotherapy information is coming too fast and needs to be simplified.” This highlights the need for easy-to-understand information on cancer websites.
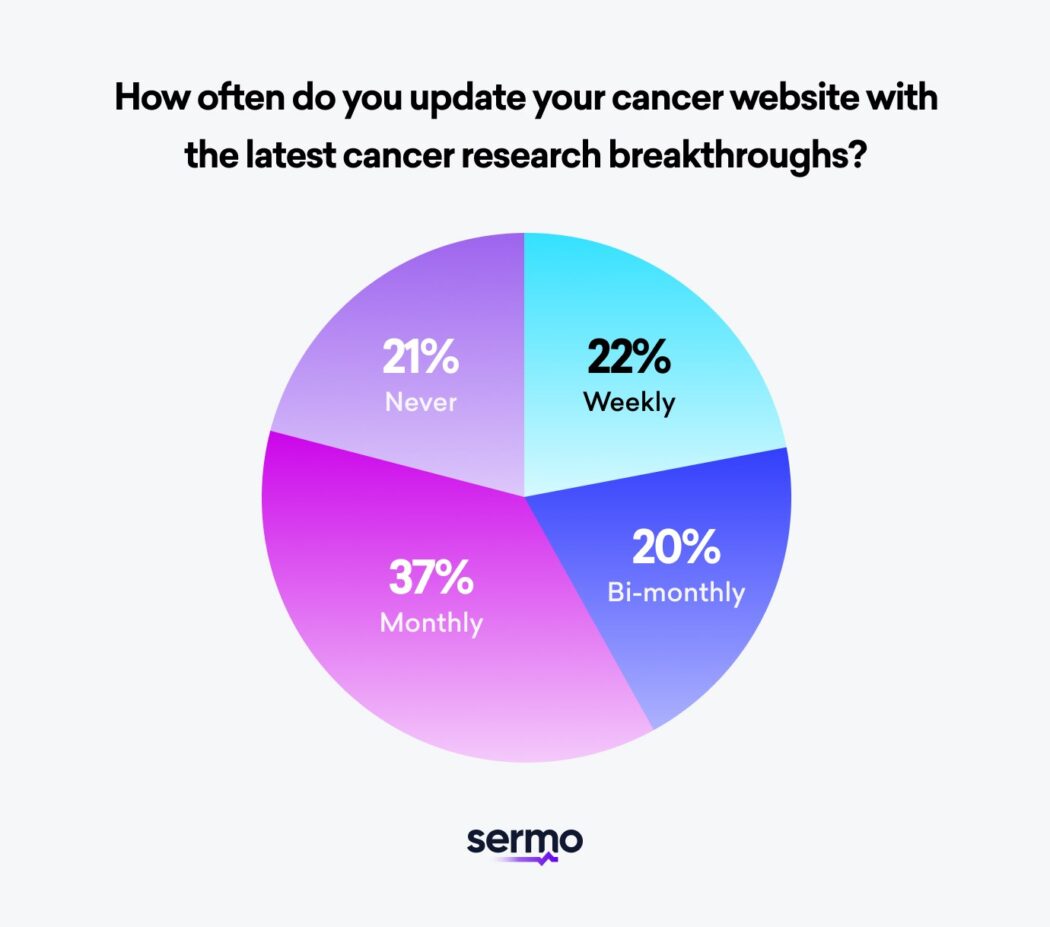
Cancer websites with updated resources containing reviews of the latest research in cancer therapy will facilitate patients’ self-education. In addition, these review articles may help your patients develop a realistic attitude toward the advances in cancer immunotherapy. Consistently publishing updated reviews of the latest cancer research boosts your center’s position as a thought leader on immune system treatment.
Use an oncology support team
Globally, there is approximately one oncologist per 100 cancer patients4. This means the average oncologist is busy. However, some patients may have questions or still need help navigating website resource pages. That’s why creating and using a dedicated support team leads to a more positive patient experience. Sermo found that 40% of oncologists reported that they have more than one person in their oncology support team.
Training and retraining members of a team on how to direct patients to resources that answer questions will reduce the time spent answering patients’ questions. It also gives doctors more time to focus on patient care.
An advanced strategy involves assembling a virtual tumor board which is a multidisciplinary team that reviews cancer diagnoses and treatment plans. This ensures the best possible cancer survival rates in the case of failed immune system response, overactive immune response, allergic reaction, or post-op autoimmune diseases. To learn more about the most effective ways to create a tumor board see our article here.
Get a physician support team
The average oncologist may not have time to consistently watch the news to stay updated on the latest cancer research breakthrough. Joining Sermo’s physician community will help you stay connected and updated on current cancer treatment advances that positively affect your patient outcomes. You can also share your learnings and hear from peers about how they handle and overcome specific clinical challenges in cancer care.
Frequently asked immunotherapy questions
What is immunotherapy and how does immunotherapy work?
Immunotherapy is a medical treatment that employs a patient’s immune system to fight cancer. Immunotherapy can boost or change how the immune system works so the immune system detects and attacks cancer cells while protecting essential functions of immune cells and healthy cells.
Is immunotherapy painful and does immunotherapy have side effects?
Immunotherapy can cause side effects. Many side effects happen when an overactive immune response also acts against body tissue, healthy cells, or beneficial immune cells.
Depending on multiple factors and the types of cancer, patients may have different side effects. The major factors are if it’s an advanced cancer, your innate immune system, and the specific immunotherapy treatment you get. Immunotherapy protocols can last a long time.
Common side effects are pain, swelling, soreness, rash, flu-like systems, congestion, and diarrhea. In very rare cases, life-threatening side effects can appear such as colitis or hepatitis.
Immune system side effects can manifest at any stage during or after treatment. Doctors and nurses cannot predict the occurrence and severity of these side effects with certainty. Therefore, regularly talking with a cancer physician or healthcare professional is crucial to gain awareness of the signs to watch out for and the steps to take if issues arise.
How is immunotherapy administered?
Immunotherapies are administered through various methods, including intravenous injection, subcutaneous injection, or intramuscular injection. In certain cases, specific types of immunotherapy can be delivered directly to the body cavity where the tumor cells are located. The type of administration will vary according to many factors including the patient’s t cells, b cells, cancer cells, inflammatory response, tumor markers, t lymphocytes, b lymphocytes, type of cancer and innate immunity.
What is the difference between immunotherapy and chemotherapy?
Chemotherapy, also known as “chemo,” is a medical treatment that uses drugs to directly kill cancer cells. This treatment method targets fast-growing tumors by attacking all rapidly-dividing cells in the body. Chemotherapy can be used on its own or in combination with surgery, radiation therapy, or immune system treatments.
Unlike chemotherapy, which acts directly on cancerous tumors, immunotherapy treats patients by acting on their immune system. Immunotherapy can boost the immune response in the body as well as teach the immune system how to identify and destroy cancer cells.
To destroy cancer cells, chemotherapy attacks rapidly dividing cells in the body, including both cancerous and non-cancerous cells like hair follicles and the gut lining. Hair loss, fatigue, and nausea are well-known side effects. In contrast, immune system therapies can lead to potential side effects resulting from an overstimulated or misdirected immune response, ranging from mild to severe, and in certain cases, posing a life-threatening risk.
What types of cancer can immunotherapy be used for?
Currently, the FDA has approved immunotherapies to treat many different types of cancer with clinical trials of more drugs on the way. Currently, there are immune system treatment options for advanced solid tumors, B-cell lymphoma, bile duct cancer, bladder cancer, breast cancer, cervical cancer, colorectal cancer, esophageal cancer, head cancer, neck cancer, Hodgkin lymphoma, kidney cancer, leukemia, liver cancer, lung cancer, melanoma, mesothelioma, multiple myeloma, non-Hodgkin lymphoma, prostate cancer, skin cancer, soft tissue sarcoma, stomach cancer and endometrial cancer.
What are other cancer treatments?
There are other cancer treatment options to consider with patients. Some of the most promising options to treat cancer are photodynamic therapy, laser therapy, targeted therapy, hormone therapy, and radiation therapy.
Are you part of a physician community?
Sermo provides access to a global online community of oncologists and other verified doctors.
Collaborate with oncologists from around the world on unique clinical situations, access physician-only resources and get invited to earning opportunities when you join Sermo for free today.